Main content
In this overview, we discuss various industrial disasters that affected the lives of many as well as individual exposure to toxins, either accidental or intentional. All have a dramatic effect on (planetary) health as well as a socio-economic impact that may result from environmental pollution or persisting disability. Lastly, we highlight the main issues in obtaining financial compensation.
Mass exposure – industrial disasters
The bhopal gas tragedy / disaster – the world’s worst industrial disaster
On the night of 2-3 December 1984, a gas leak occurred at the Union Carbide Indian Limited pesticide plant in Bhopal, Madhya Pradesh, India. Over 500,000 people were exposed to methyl isocyanate (MIC) gas, the worst industrial disaster ever. The official immediate death toll was 2,259. In 2006, the Government of Madhya Pradesh stated that the leak caused over 550,000 injuries including 38,000 temporary partial injuries and 3,900 severely and permanently disabling injuries.(1,2)
The initial effects were coughing, severe eye irritation, and breathlessness. Children were more affected as the gas tends to fall toward the ground.
The following day, thousands had died mostly because of choking, circulatory collapse and pulmonary oedema. Autopsies revealed renal injury, cerebral oedema, liver necrosis and necrotising enteritis.
In the immediate aftermath, the health services became overwhelmed; there was no plan on how to deal with a disaster of this magnitude and there was no awareness of appropriate treatment methods. Mass funerals and cremations took place. 170,000 people were treated in hospital or temporary facilities. Trees in the vicinity became barren and thousands of animals were collected and buried. Long-term effects include eye disease (cornea scars, opacities), respiratory disease (pulmonary fibrosis), neurological disorders (memory loss), psychological problems (Post Traumatic Stress Syndrome: PTSS), cancers, and child health damage (risk of peri- and neo-natal death). The stillbirth rate was up by 300% and neonatal mortality by around 200%. Those who did not die suffered severe socioeconomic consequences in addition to health problems.(1,2)
Extensive litigation followed; Union Carbide agreed to pay USD 470 million for damages and was ordered to fund a hospital in Bhopal to specifically treat victims of the disaster at a cost of USD 17 million. The Indian Supreme Court ordered the Indian Government to purchase a group medical insurance policy to cover 100,000 persons who might later develop symptoms.(1)
Yellow cake (‘’urania’’)
Yellow cake is a type of uranium concentrate powder that is a step in the processing of uranium before fuel fabrication or uranium enrichment. It is produced by in situ leaching, in which acid, alkaline and peroxide solutions are pumped through the uranium deposit. Yellow cake is what remains after drying and filtering.(3) It is used for uranium fuel for nuclear reactors. Uranium can be enriched to the isotope U-235. Low-enriched uranium, with up to 20% of U-235, is suitable for electro-power reactors. Highly enriched uranium (>20% U-235) is suitable for compact nuclear reactors used in naval warships and submarines. Uranium with levels of U-235 > 90% is suitable for nuclear weapons.(4)
Niger has the world’s fourth largest uranium reserves. When France discovered uranium in its former colony, it was felt as a blessing for the country, which ranks 187 out of 188 countries on the United Nations Development Index. Areva, a French state-owned mining company, extracted uranium in open pits as well as in mines. Niger has benefited only marginally but suffers from tremendous pollution, leading to chronic exposure to radiation in miners who work without even minimal personal protection such as face masks. The long-term effects are not well known, but deformed babies, high death rates, and lung cancer are among the commonly perceived consequences.
Yellow cake mining in Niger leaves Niger in the dark (90% have no electricity), while in France one in three light bulbs is lit thanks to Niger’s uranium being used in nuclear energy: a classical example of ruthless (colonial) exploitation of a poor country’s resources.
Nuclear radiation
The Chernobyl disaster (Ukraine, 1986) occurred because of poor maintenance and mismanagement. Thirty operators and firemen died within 3 months as a result of the accident. Around 20 people died as a result of acute radiation syndrome. More than 335,000 people were evacuated. A large cloud of radioactivity spread over Europe across an area of 160,000 km2 where radioactive caesium (137Cs), one of the common fission products of the fission of U-235, was detected in the air.[5,6] For some time, the consumption of crops of vegetables was discouraged. Despite the exposure to high levels of radiation, no major long-term health effects were noted.[7] The feasibility of resettlement and agriculture are subject to examination; in 2011 Chernobyl was declared a tourist attraction. Wildlife is thriving in the absence of humans despite exposure to radiation.
The Fukushima disaster (Japan, 2011) was triggered by a tsunami caused by an earthquake off the coast of Japan. The tsunami destroyed the reactor’s cooling system. No casualties resulted directly from exposure to radiation; all deaths were due to the impact of the tsunami. A large area surrounding the nuclear plant, with a diameter of 20 km2, was evacuated, including 154,000 people. Large quantities of radioactive water were released into the Pacific ocean, which continued for years thereafter.[8] The incident caused a great scare world-wide and increased existing negative sentiments against the use of nuclear energy. In Germany, former chancellor Merkel put in place the ‘’Atomausstieg’’ (nuclear power phase-out), a decision that has serious consequences now that the supply of Russian gas as a source of energy is decreasing because of the Ukraine war.
The shell oil disaster in nigeria
Since 1958, oil has been commercially produced by the Shell oil company in the Niger River delta in Nigeria. Multiple oil leakages due to poor maintenance and in some areas, sabotage, have occurred with deleterious impacts on farmlands, fishponds, rivers, and residential areas. While the local population hardly benefits from the oil production, they suffer from a lack of clean drinking water, poor housing, poor health, and poor health care. It is a matter of a handful of poor farmers fighting for justice against a powerful multinational and a dysfunctional Nigerian Government, which has failed to regulate the oil industry and protect the rights of the local population. In 2020, Amnesty International and other NGOs reported that no more than 11% of polluted areas had been cleaned. In 2021, a Dutch court ruled that Shell is liable for damages and must offer compensation. In addition, Shell needs to do more to prevent further damage and renew pipes and other infrastructure.[9]
Mass exposure – by ingestion – the toxic oil syndrome (bad olive oil)
In 1981 in Spain, 25,000 people in or around Madrid became ill within a short period of time, and hundreds died. About 100,000 were exposed to a toxin, long-term mortality is estimated at 5000 people, and 20,000 have survived with poor quality of life. (10,11,12) The cause was shown to be rapeseed oil adulterated with 2% aniline (phenylamine) and sold illegally by street vendors as “olive oil”.(11) It started with flu-like symptoms and a morbilliform rash. In the first months, deaths were due to a chemical pneumonia with very high eosinophilia. Later, deaths were mainly from unremitting pulmonary hypertension and chronic cor pulmonale (right-sided heart failure due to pulmonary hypertension); many developed a scleroderma-like illness with neuromuscular and cutaneous manifestations. Studies showed degeneration of the conduction system leading to conduction disturbance, arrhythmias and sudden death. In addition, fibromuscular dysplasia in the coronary arteries could lead to ischaemia. (11)
The implication for rapeseed caused considerable discussion as this oil was thought to be beneficial for lowering cholesterol. While rapeseed oil has been used for centuries in the Orient, it was only introduced in the Western world several decades ago. However, growing rape plants and producing rapeseed oil has developed into a multibillion dollar industry. The result was a bitter trade and tariff dispute between French and Canadian farmers; the Canadian product was called canola oil and contained only a few percent of erucic acid, the perceived culprit compound of rapeseed oil. In 1989, after the longest trial in Spanish history, judges dismissed charges for murder or intentional injury against distributors; some were given prison sentences for importing and tampering, but many of the accused were acquitted, causing an uproar. (10)

Mass exposure – arsenic in the environment
The WHO estimates that > 200 million people across 70 countries are chronically exposed to concentrations of inorganic arsenic (As) in drinking water.(13) Bangladesh, India, Taiwan and Peru are among the worst affected countries. (14) The health risks include lung, bladder and skin cancer, ischemic heart diseases, and skin lesions. There is increasing evidence for the development of neurodevelopmental deficits in children and adolescents after exposure to As in drinking water as well as to cadmium (Cd). It is not clear to what extent genetic polymorphisms play a role that could result in differences in detoxification enzymes, DNA repair, and tumour suppression proteins. Epigenetics may play a role whereby arsenic exposure induces different gene expression leading to predisposition to cancer and other diseases. (15)
Individual exposure
Acetic acid intoxication – a culturally determined intoxication
Concentrated acetic acid (also called glacial acetic acid) has an 80-85% content of acetic acid (also known as ethanoic acid) and needs to be diluted to 4% before consumption, e.g. as a salad dressing; it has a pungent, vinegar-like odour. In a report from 1977, 100-200 cases of acute intoxication with concentrated acetic acid were reported to occur annually in Surinam in a population of 350,000. (14) Similar cases (25-30 annually in a population of 160,000) were reported in 1982 from Curacao, Netherlands Antilles. (15) The female to male ratio was 3:1 to 5:1. In both countries, the cases mainly involved suicide attempts.
The clinical features include erosions on the mucosa of mouth, oesophagus and stomach. In severe cases, haematemesis occurs with perforation of the oesophagus, stomach, or jejunum, leading to mediastinitis or peritonitis. Aspiration leads to bronchopneumonia. General complications include haemolysis, renal failure, and circulatory insufficiency, likely to be caused by myocarditis. Intravascular coagulation has been described. Long-term complications include oesophagus stenosis leading to aspiration pneumonia; repeated dilatation of the oesophagus may be needed. Treatment is supportive. Antibiotics are indicated for 4-8 weeks if perforation is suspected. The role of steroids in the prevention of long-term stenosis is controversial. The increasing number of cases was a reason for calling for political action to prohibit the sale of concentrated acetic acid.(17)
The softenon™ scandal
Softenon™ (thalidomide) had been used world-wide since 1957 for sleeping problems and as a sedative and pain killer. Later, it was also used to treat pregnancy-induced vomiting. In 1961, it became clear that it caused severe abnormalities in newborns. More than 100,000 children have been born with abnormalities of the eyes, kidneys, or genitals, and in particular short or absent limbs (focomelia).(18) Before Softenon™, focomelia was a rare condition; it was caused by inhibition of angiogenesis – the growth of blood vessels of limbs. In the late 1980s, the drug was reintroduced for several indications, including mouth ulcers in HIV infection, leprosy, Behcet’s syndrome and other rheumatic diseases; inhibition of angiogenesis was thought to be of importance in the treatment of cancer. It is on the WHO list of essential medicines.(19)
Only in 1982 did Chemie Grünenthal (Stolberg, Germany) apologize for the production of Softenon™. There is information that suggests that, as early as 1959 (two years before it was banned), the side-effects were already known but were covered up. The media played an important role in finding the truth. The scandal led to more stringent rules for drug research and registration.(18)
Domestic smoke
In low- and middle-income countries (LMICs), many households use a mixture of fuels for cooking, including charcoal and wood. In addition, various other smoky means of lighting, such as paraffin, tin lamps and candles, are used. This causes exposure to particulate material by inhalation. If these particles are larger than 0.5 mm in diameter, they are deposited in the muco-ciliary lining of the trachea and bronchi. This mucus is constantly swept towards the throat, where it is swallowed.(20,21)
The effect of smoke on the ciliary function has been the subject of study. One study from Malawi suggested that smoke exposure is a risk factor for reduced lung function and COPD. This mechanism may be similarly impaired by cigarette smoking, which is an important risk factor for pneumonia. This has not been studied in LMICs, where smoking is less common. Domestic smoke is also a risk factor for lung carcinoma of the lung, nasopharynx and oesophagus, as was shown in a study from Zambia. (22,23) In a review paper, Gordon et al describe the scope of the problem and outstanding issues for research. Solutions that have been proposed are the use of high-efficiency cookstoves and the use of charcoal instead of wood, which reduces the exposure to smoke. Outdoor cooking is promoted, which also reduces the occurrence of burn injuries.(22)
The result of exposure to smoke and large particles can clearly be seen in fluid obtained from a bronchoalveolar lavage (Figure 2).

Panel A. Bronchoalveolar washing from individuals exposed (left) or not (right) to domestic smoke.
Panel B. Domestic smoke exposure: Macrophages in a BAL samples have phagocytosed numerous carbon particles.
Panel C. No domestic smoke exposure: few carbon particles have been phagocytosed.
Para-phenylene diamine poisoning (ppd) – a cosmetic product that may be used to commit suicide
Para-phenylene diamine (PPD) has traditionally been used as a dark-coloured hair dye. It may be used alone or in combination with colouring extracts such as henna for dyeing the hair or the skin (Figure 3,4). It is popular in African countries such as Sudan, Morocco, and Egypt and is also used in India. Chronic as well as acute intoxications have been described. In the ENT hospital in Khartoum, Sudan, each year 300 cases are seen with 10% mortality. (24) Acute intoxication occurs because of accidental or intentional (suicidal or homicidal) exposure to pure PPD. Suicide accompanied by filicide has been reported; a Sudanese woman killed herself and poisoned her 4 children of whom 1 died, 1 recovered after dialysis and 2 others recovered without intervention.(25) In Sudan, PPD is readily available on the local market and is very cheap. The clinical syndrome after ingestion includes laryngeal oedema, rhabdomyolysis and subsequent renal failure, neurotoxicity (paraplegia) and toxic hepatitis (Figure 5).
There is no antidote and management is supportive.



Lead poisoning – occupational and recreational exposure
Lead poisoning commonly results from occupational exposure in workers employed in a battery recycling plant; other sources are the use of Ayurvedic products to which lead is added or opium-chewing.(26) Other less common cases include a history of gunshot and residual bullets in the bone marrow. Another case had a history of prolonged usage of ritual pills and holy paper incineration. Clinical features include colicky abdominal pain, renal failure, and anaemia.
In acute intoxication, the classic form of lead neuropathy may present as weakness of the wrist and finger extensors, and later spread to other muscles. There is only minimal sensory involvement.
Chronic exposure leads to a more typical toxic neuropathy with distally accentuated sensory and motor involvement. Axonal degeneration may occur. In children, there may be a link with neuropsychological disorders.
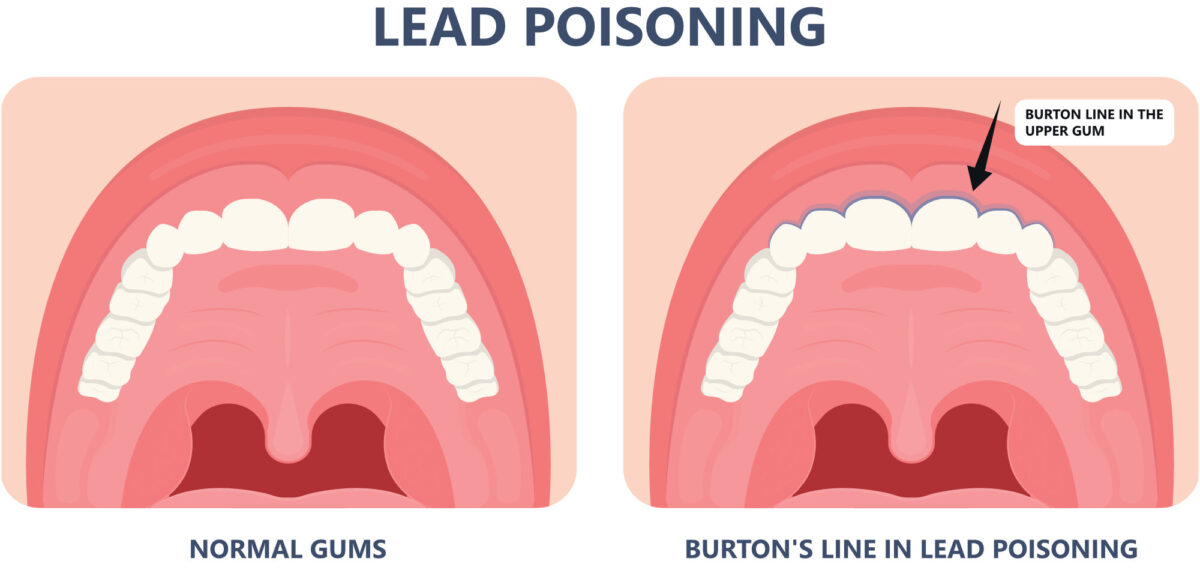
On clinical examination, Burton’s line should be looked for [Figure 6]. This is the result of a reaction between lead in the blood and degradation products of oral bacteria. Management includes immediate termination of exposure; chelation therapy to bind and remove lead from the blood should be tried in acute poisoning but is controversial in neuropathy.(27,28)

Carbon monoxide (co) poisoning
At least 21 teenagers died in a tavern in East London, South Africa, on an early Sunday morning in late June 2022. As the Electricity Supply Commission (ESCOM) of South Africa is unreliable in providing an uninterrupted electricity supply, private houses or businesses often have to depend on their own generator. In this case, a petrol generator was placed inside the tavern that had all its doors locked. It is likely that carbon monoxide accumulated, which has no smell, taste or colour and causes headache, dizziness, coma and death.(29)
CO binds to haemoglobin with much greater affinity than oxygen, thus reducing the oxygen carrying capacity of the blood. Diagnosis is done by measuring the carbon monoxide level in the blood. Standard pulse oximetry (SpO2) not reliable, as it cannot differentiate between carboxyhaemoglobin and oxyhaemoglobin. Treatment is with high-flow oxygen through a non-rebreather mask; hyperbaric oxygen may be considered in severe cases.
Long term sequelae include myocardial toxicity and neuropsychiatric syndrome with personality changes, focal neurological deficits, and cognitive effects.
It is sad to realize that, even in South Africa, mismanagement and corruption have affected safe and uninterrupted electricity supply by ESCOM, leading to tragedies such as this one. In general, adequate ventilation and well-tuned engines, such as generators that burn clean with minimal CO production, are helpful in preventing such disasters.
* At the time of print, other factors such as combined exposure to methanol or another unidentified substance were still under investigation.
Microplastic – the new threat to human and animal health?
World-wide pollution with plastic is a major reason for concern, and not only for the environment, as (macro) plastic has been demonstrated in various animals resulting in serious morbidity such as gastrointestinal obstruction. Potential toxic effects for humans are not known. Recently, it became possible to measure microplastic in human blood samples that probably have been absorbed from the gut.(30) The mean concentration in the blood was 1.6 microgram per millilitre and the particle size varied from 700 nanometre to 0.5 millimetre. It is estimated that, during life, an individual consumes the equivalent of 3 credit cards of plastic. The significance of these findings is not clear. The methodology used is still a subject of study, but research is focused on the potential role of microplastics in inflammatory processes, such as inflammatory bowel disease (Crohn’s disease, ulcerative colitis) or irritable bowel syndrome.(30,31)
References
- Varma R, Varma DR. The Bhopal disaster of 1984. Bulletin of Science 2005;25:37-45.
- https://en.wikipedia.org › wiki › Bhopal_disaster
- Gil, L. Uranium leaching: How yellow cake is made. IAEA Bulletin (online) 2018;59 iss 2; 22-23.
- https://en.wikipedia.org › wiki › Yellowcake
- https://en.wikipedia.org › wiki › Chernobyl_disaster
- Health effects of the Chernobyl accident and special care programmes. Report of the Chernobyl Forum, expert group “Health”, World Health Organization, 2006 (ISBN: 9789241594172)
- https://www.world-nuclear.org/search.aspx?searchtext=chernobyl
- https://en.wikipedia.org › wiki › Fukushima_nuclear_di.
- https://www.amnesty.org/en/latest/press-release/2011/08/un-confirms-massive-oil-pollution-niger-delta/
- https://www.reuters.com/world/europe/fake-olive-oil-scandal-that-caused-spains-worst-food-poisoning-epidemic-1981-2021-10-19/
- James TN. The Toxic Oil Syndrome. Clin Cardiol 1944;17;463-470.
- WHO Report: Toxic Oil Syndrome – Ten years of progress. http://www.euro.who.int/document/e84423.pdf
- Wasserman GA, Liu X, Perez F, et al. A Cross-Sectional Study of Water Arsenic Exposure and Intellectual Function in Adolescence in Araihazar, Bangladesh. Environ Int. 2018 Sep; 118: 304–313.
- Lan C, Yu H, KoY. Chronic arsenic exposure and its adverse health effects in Taiwan: A paradigm for management of a global environmental problem. Kaohsiung J Med Sciences. First published: 05 July 2011. https://doi.org/10.1016/j.kjms.2011.05.009
- Minatel BC, Sage AP, Anderson C, et al. Environmental arsenic exposure: From genetic susceptibility to pathogenesis (Review). Environ Int . 2018 Mar;112:183-197. doi: 10.1016/j.envint.2017.12.017. Epub 2017 Dec 22.
- De Vries RRP, Sitalsing AD, Schipperheyn JJ, Sedney MI. Klinische aspecten van azijnzuurintoxicatie. Ned T Geneesk 1977;121; 862-866.
- Nossent JD, Vismans FJFE. Azijnzuur intoxicatie op Curacao. Ned T Geneesk 1982;126; 1180-1183.
- https://en.wikipedia.org › wiki › Thalidomide
- World Health Organization (2019). “World Health Organization model list of essential medicines: 21st list 2019”. hdl:10665/325771.
- Fullerton DG, Jere K, Jambo K, et al. Domestic smoke exposure is associated with alveolar macrophage particulate load. Trop Med Int Health. 2009 Mar;14(3):349-54. doi: 10.1111/j.1365-3156.2009.02230.x
- Fullerton DG, Suseno A, Semple S, et al. Wood smoke exposure, poverty and impaired lung function in Malawian adults. Int J Tuberc Lung Dis. 2011 Mar;15(3):391-8. PMID: 21333109
- Gordon SB, Bruce NG , Grigg J, et al. Respiratory risks from household air pollution in low and middle income countries Lancet Respir Med 2014 Oct;2(10):823-60. doi: 10.1016/S2213-2600(14)70168-7. Epub 2014 Sep 2.
- Kayamba V, Bateman AC, Asombang AW, et al. HIV infection and domestic smoke exposure, but not human papillomavirus, are risk factors for esophageal squamous cell carcinoma in Zambia: a case-control study. Cancer Med 2015 Apr;4(4):588-95. doi: 10.1002/cam4.434. Epub 2015 Jan 30.
- Hooff GP, van Huizen NA, Meesters RJW, et al. Analytical investigations of toxic p-phenylene diamine (PPD) levels in clinical urine samples with special focus on MALDI-MS/MS. Plos One 6(8): e22191
- Abdelraheem MB, Elbushra M, Ali el-T, et al. Filicide and suicide in a family by paraphenylene diamine poisoning: a mother who committed suicide and poisoned her four children of which one died. Toxicol Ind Health 2014 Sep;30(8):679-82. doi: 10.1177/0748233712448118. Epub 2012 Dec 6.PMID: 23222690
- Ciocan C, Mansour I, Beneduce A, et al. Lead poisoning from Ayurvedic treatment: a further case. Med Lav 2021 Apr 20;112(2):162-167. doi: 10.23749/mdl.v112i2.10576.
- Wiwanitkit VJ. Lead intoxication: a summary of the clinical presentation among Thai patients. Biometals 2006 Aug;19(4):345-8. doi: 10.1007/s10534-004-2994-x.
- Thomson RM, Parry GJ. Neuropathies associated with excessive exposure to lead. Muscle Nerve 2006 Jun;33(6):732-41. doi: 10.1002/mus.20510.
- https://www.citizen.co.za › News › South Africa Enyobeni: Carbon monoxide poisoning likely cause of deaths.
- Kruimeltjes in het bloed. NRC Newspaper W6-7, Saturday 18 and Sunday 19 June 2022
- Xiao Zhi Lim. Microplastics are everywhere — but are they harmful? www.nature.com/articles/d41586-021-01143-3


















































