Main content
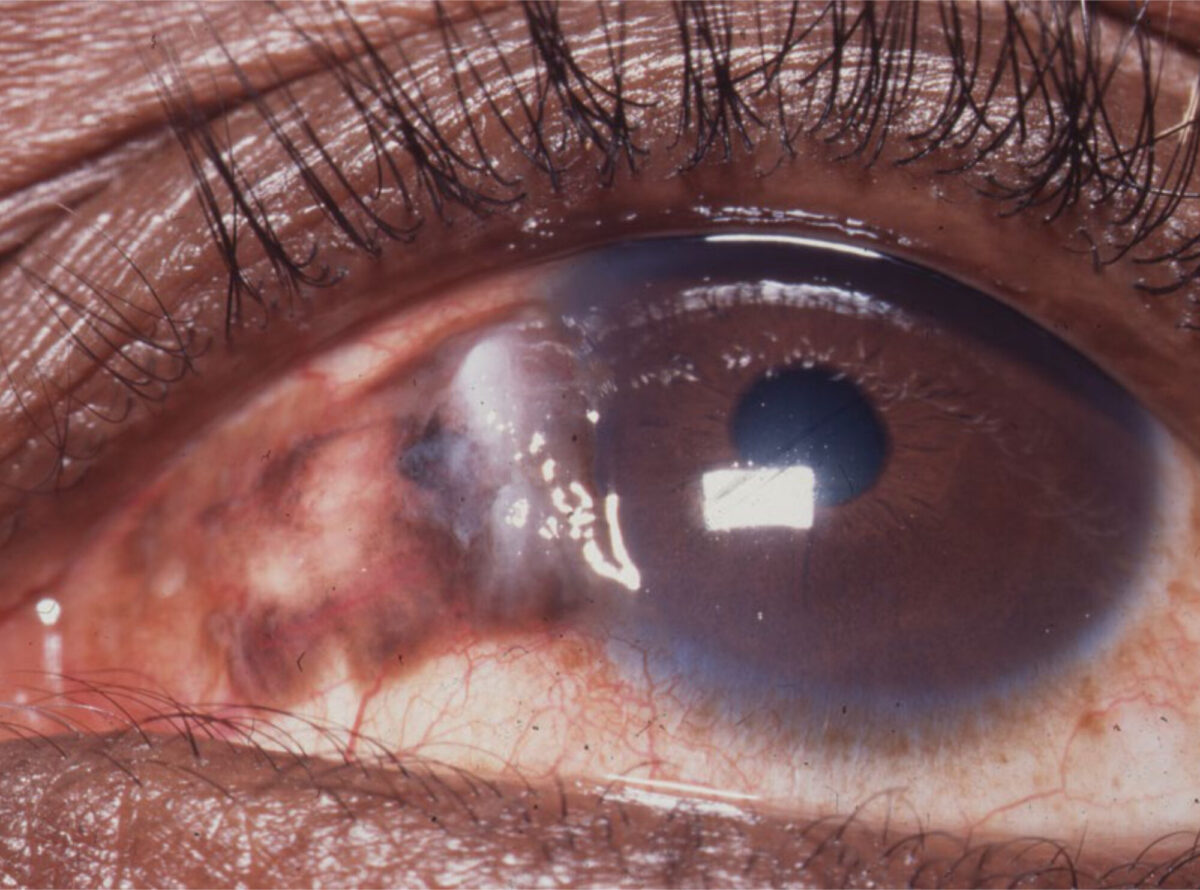
Imagine, you are a general practitioner in a middle-sized city somewhere in sub-Saharan Africa. On Monday morning your first patient in the Out Patient Department is a 33-year-old male with, since two weeks, the symptoms of herpes zoster ophthalmicus on the left side. He cannot close his left eye anymore due to scar formation of the upper eyelid, his eye is painful, red and filled with puss, the vision in this eye is markedly reduced. The second patient is a 40-year-old woman with, since several months, a conjunctival growth on the right eye. The third patient is a 29-year-old male with, since several weeks, a strange, thickened dark red upper eyelid of the left eye. The eyelid is not painful. He has dark red patches in his oropharynx. The fourth patient, a 36-year-old woman, has been put on HAART recently as she was found to be HIV positive. She is complaining of loss of vision.
Different times
30 years ago it was very rare to start the week in the OPD like this. However, with the arrival of HIV opportunistic infections like herpes zoster ophthalmicus (patient 1) and neoplasmata like squamous cell carcinoma of the conjunctiva (patient 2) and Kaposi sarcoma (patient 3), are nowadays common in relatively young patients. And since the introduction of Highly Active Antiretroviral Treatment (HAART) in 1996 new phenomena like Immune Recovery Uveitis (patient 4) have appeared (see article Meenken & van den Horn in this MT bulletin). Worldwide more than 35.3 million people have been infected with HIV, the greater part in sub-Saharan Africa (25 million), Asia (4.8 million) and North America/Western Europe (2.1 million). In lower-income countries it is the second cause of death after lower respiratory infections. Adnexal and orbital complications affect more than 25% of untreated HIV-positive patients and could be the presenting sign of the disease. Keratoconjunctivitis sicca occurs in 10 to 20% of patients and in more advanced stages of the disease posterior segment manifestations like retinal microvasculopathy and cytomegalovirus (CMV) retinitis are seen in some areas in 40-50% of patients.
Opportunistic infections
Eye diseases diminish the quality of life of patients suffering from AIDS. For the general practitioner it is important to recognize that an infection can be opportunistic, due to AIDS. As many general practitioners are the first doctors patients visit they are the ones who diagnose the disease and who decide on therapy and referral. In this paper some tools are presented to recognize HIV related eye diseases and to facilitate treatment and/or referral.
Two important skills are necessary to fulfil this task: knowledge and examination skills. The general practitioner should have knowledge about which opportunistic infection fits into the picture of a certain level of immunodeficiency. And the general practitioner should be capable of performing a basic eye examination. HIV is acting by reducing the number of CD4 cells, eventually leading to deep immune incompetence, which paves the way for opportunistic infections and neoplasmata.
In diagnosing an opportunistic infection a handy tool is the hand ophthalmoscope. Floaters can be recognized easily(see article Hardus and others in this journal). Therapy depends on the availability of drugs. In individuals with advanced immunodeficiency more aggressive therapy is mandatory as they have an increased risk of permanent vision loss.
Herpes zoster
A patient with herpes zoster ophthalmicus could benefit from acyclovir (800 mg five times daily) or valaciclovir (1000 mg three times daily), topical calamine lotion or emollient, potassium permanganate soaks, systemic antibiotics in case of secondary infection and analgesics like indomethacin (50 mg three times daily), while amitryptillin (75-150 mg at night) and carbamazepine (100 mg once or twice daily) can reduce post herpetic neuralgia. Local therapy for cornea exposure due to a retracted upper eyelid could consist of eye ointment and a tarsorraphy.
Kaposi
In case of a Kaposi sarcoma of the eyelid and conjunctiva there are more Kaposis in the mouth. Median survival in sub-Saharan Africa is 3.5 months. Treatment is, in the first place, to start HAART as soon as possible as it greatly improves the chance of survival. Surgical excision is sometimes possible, but as Kaposi sarcoma is a heavily vascularized tumour this can be difficult. Radiotherapy and intralesional vinblastine chemotherapy are other options.
Conjunctival growth
The differential diagnosis of a conjunctival growth is (apart from a few other rare tumours like non-Hodgkin lymphoma, pyogenic granuloma after trauma and papilloma) pinguecula (harmless hyalin degeneration), pterygium (from the conjunctiva spreading “wing” over the cornea with parallel blood vessels giving rise to astigmatism and eventually covering of the pupil) and conjunctival intraepithelial neoplasia leading to squamous cell carcinoma of the conjunctiva. Squamous cell carcinoma of the conjunctiva must be excised completely with a free zone around the process of at least 2 mm as recurrences can be very aggressive. If possible the whole area is treated with double freeze-thaw cryotherapy. An alternative is application of 5-fluoro-uracil 1% eye drops four times daily during four days followed by ten days rest and reinstallation of 5-fluoro-uracil 1% four times daily. In case of metastasis the first stations are the submandibular- and pre-auricular lymphnodes. If the CD4 count is below 200 patients are more likely to suffer from intra-ocular infections. Those infections reduce the visual acuity and can be diagnosed by funduscopy. Look for local and systemic signs of the infections of table 1. AIDS is still a deadly disease. In general, prompt diagnosis of HIV and timely start of treatment with HAART is essential to improve the condition of the patient.


| CD4 < 500 | Herpes zoster ophthalmicus Kaposi sarcoma Lymphoma Squamous cellcarcinoma conjunctiva |
| CD4 < 200 | Tuberculosis Toxoplasmosis Fungal infections like Coccidioidomycosis, Cryptococcosis, Histoplasmosis, Pneumocystis jirovecii |
| CD4 < 100 | Cytomegalovirus retinitis, Herpes zoster virus retinitis Mycobacterium avium complex infection Microsporidiosis Progressive multifocal leucoencephalopathy Retinal/conjunctival microvasculopathy |
Acknowledgements
Many thanks to Hans van den Horn and Ina Meenken, ophthalmologists, for reviewing this manuscript.
References
- Cunningham ET Jr, Margolis TP, Ocular manifestations of HIV infection. N Engl J Med 1998;339:236-44.


















































