Main content
In everyday clinical practice, in high-income countries (HICs) as well as low- and middle-income countries (LMICs), medical imaging is important in making a diagnosis. Particularly in LMICS, in most settings, patient assessment in internal medicine is done through carrying out a thorough clinical assessment, laboratory tests and imaging. In most peripheral settings, this would be limited to a chest x-ray, an abdominal x-ray and ultrasound examination. At the central level, a CT scan or an MRI scan may be available. A differential diagnosis is then made against the background of knowledge of the local epidemiology of most common conditions. Obviously, in LMICs, this differs between, say, Sudan, Papua New Guinea and Peru.
Clearly, other specialties have different priorities in imaging, as in orthopaedics and obstetrics and gynaecology (O&G), but the available tools are basically the same. Ultrasound is well integrated in daily practice for example in O&G and in urology.
In recent years new imaging tools have become available, and old tools have been adapted to be used in a LMIC setting. In this paper, an overview is given of two such important developments: portable ultrasound performed by the clinician and 3-dimensional scanning.
Ultrasound
Ultrasound is widely available in LMICs and is often performed by a radiographer, but there are few trained radiologists. The quality and interpretation of the scan depends on the radiographer’s skills acquired by training and experience as well as continuing education and supervision; the latter two factors are often not sufficiently addressed. Portable ultrasound machines are widely available and can be used at the bedside or in the field.
Point-of-care ultrasound (POCUS) refers to the use of ultrasound by the clinician and is performed at the bedside for diagnostic and therapeutic purposes. It helps to narrow the differential diagnosis. It is non-comprehensive in the sense that it only focuses on specific clinical questions, such as the presence of pleural fluid or post-renal obstruction as the cause of renal failure. Wider, unbiased screening e.g. the cause of abdominal pain of unknown origin is still in the domain of the diagnostic ultrasound performed by the radiology department. POCUS is increasingly used in the emergency department, clinical departments, and in the out-patient clinics in HICs.
Studies are ongoing on the evaluation of the quality of the point-of-care use by a clinician vs. regular ultrasound scanning by a radiologist. Good sensitivity (90%) and specificity (100%) were found in the evaluation of acute kidney failure in ultrasound scans performed with POCUS in an emergency department compared with ultrasound at the radiology department. In addition, the negative predictive value of 99% suggested that POCUS can serve as a tool to reduce the need for regular ultrasound scanning.[1] Recently, the use of portable ultrasound at the bedside was demonstrated in the diagnosis of Covid-19 pneumonia and daily follow-up. It was emphasised that imaging of the lung should be combined with scanning of surrounding structures such as the heart for the purpose of the differential diagnosis, and that the findings should be interpreted in combination with clinical features.[2]
As portable ultrasound machines are becoming increasingly available, POCUS should be integrated in the curriculum of clinicians who prepare to work in LMICS.[3] POCUS courses have been introduced in LMICs, for example at the level of registrars in internal medicine in Malawi (EE Zijlstra, personal communication). In this POCUS course, clinicians are trained in a two-weeks hands-on training course on the wards. Following the course, half of the departmental ultrasounds were done as POCUS.[4] It aims to enable the clinician to assess the following:
- free fluid – pleural, pericardial, ascitic
- heart function
- pneumothorax
- kidney size and brightness (points to chronic kidney disease); hydronephrosis
- deep vein thrombosis
- signs of disseminated tuberculosis
The POCUS course in Malawi is adapted to the local pathology and addresses, for example, issues in the diagnosis of tuberculosis and heart failure. There are disease-specific protocols such as FASH (focused assessment by sonography of HIV-associated extra-pulmonary tuberculosis) (Figure 1).[5]
- Cardiac (subxiphoid or parasternal long-axis), aortic and upper abdominal view to assess for pericardial effusion and abdominal lymph nodes in the upper abdominal peri-aortic region
- Right lung base to assess for pleural effusion
- Right upper quadrant (RUQ) view to assess the liver, right kidney and the space between Morison’s pouch for free fluid
- Left lung base to assess for pleural effusion
- Left upper quadrant (LUQ) view to assess the left kidney, spleen, subphrenic and splenorenal space
- Pelvic view to assess the suprapubic region, urinary bladder and rectouterine/retrovesical pouch
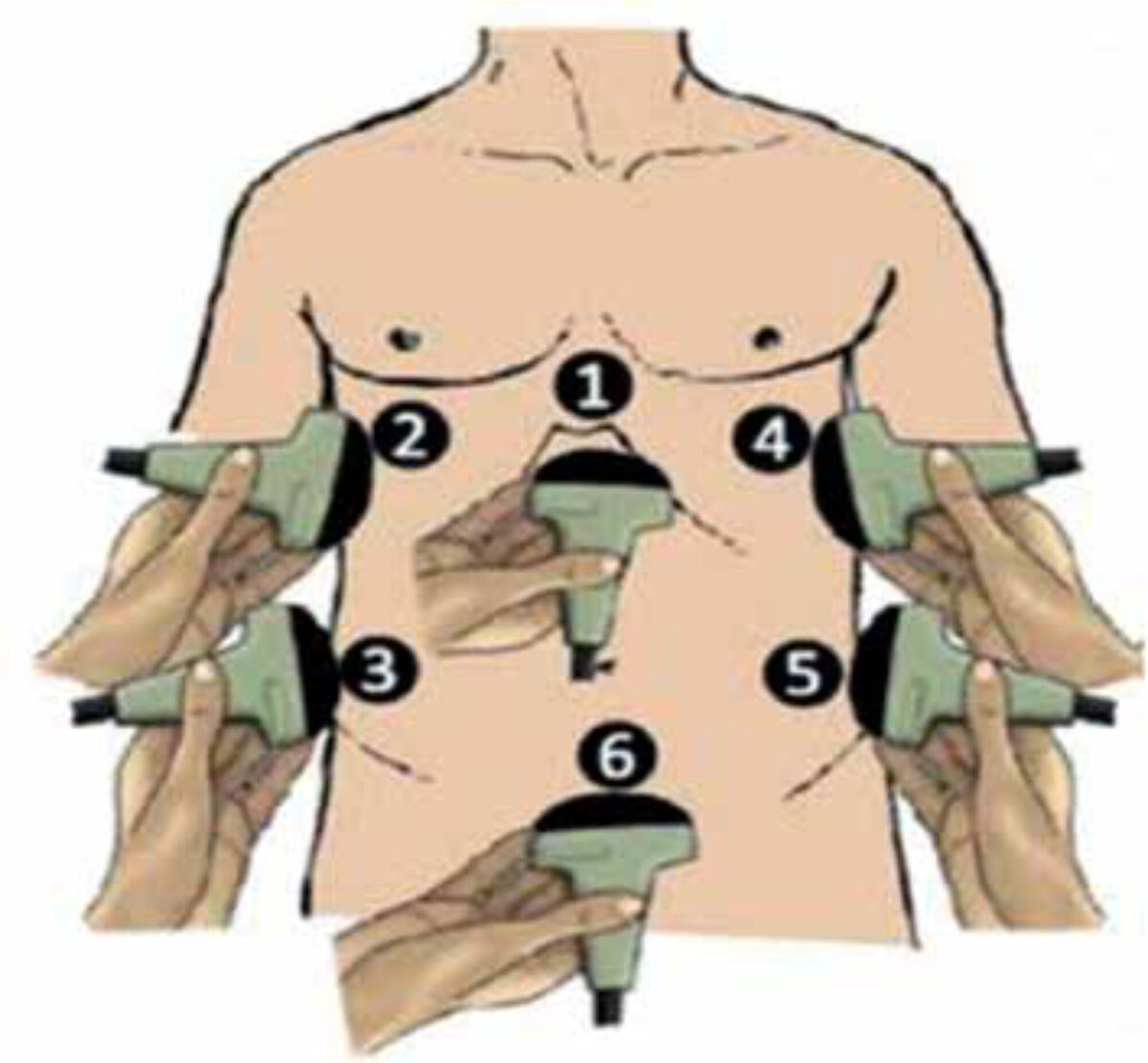
The FASH protocol helps to identify diagnostic options, e.g. an aspirate of pleural or ascitic fluid may be examined for protein, glucose and LDH levels; white blood cell count and Gram stain and stain for acid-fast bacilli, to support the diagnosis of extra-pulmonary tuberculosis.
Another protocol is CURLS (cardiac ultrasound in resource-limited settings). Here the aim is also to enable the clinician in a LMIC setting to diagnose the most important conditions that may underlie common clinical presentations such as heart failure and cardiomegaly.[7]
- pericardial effusion
- dilated cardiomyopathy
- cor pulmonale
- mitral valve disease
- left ventricular hypertrophy
There are also disease-specific protocols such as FASE (focused assessment with sonography for echinococcosis) that may be used in diagnosis and monitoring of treatment.[3]
3-dimensional scanning
3-Dimensional scanning is a novel diagnostic tool that allows assessment of abnormalities that are in or above the level of the skin. This technique has been developed in detail in oral and maxillofacial surgery for patients in whom large parts of facial structures have been removed because of (surgery for) cancer or trauma. The technique helps to construct a facial prosthesis with great accuracy that can then be printed by a 3D printer and implanted surgically with optimal fit.[8]
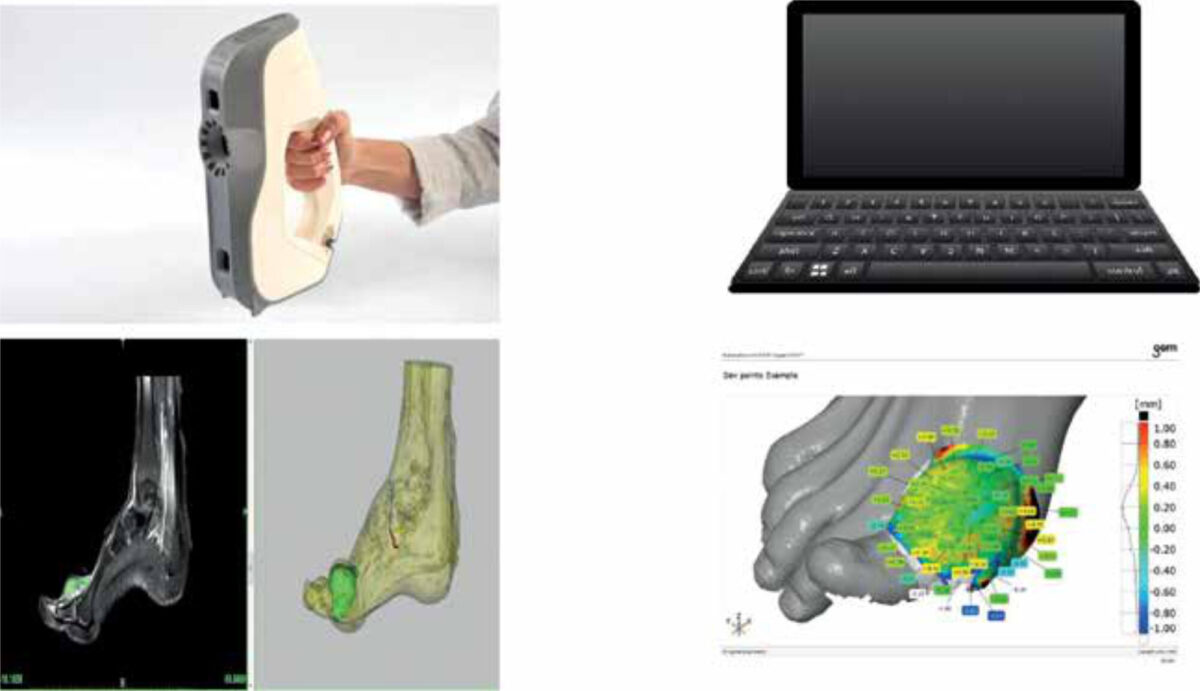
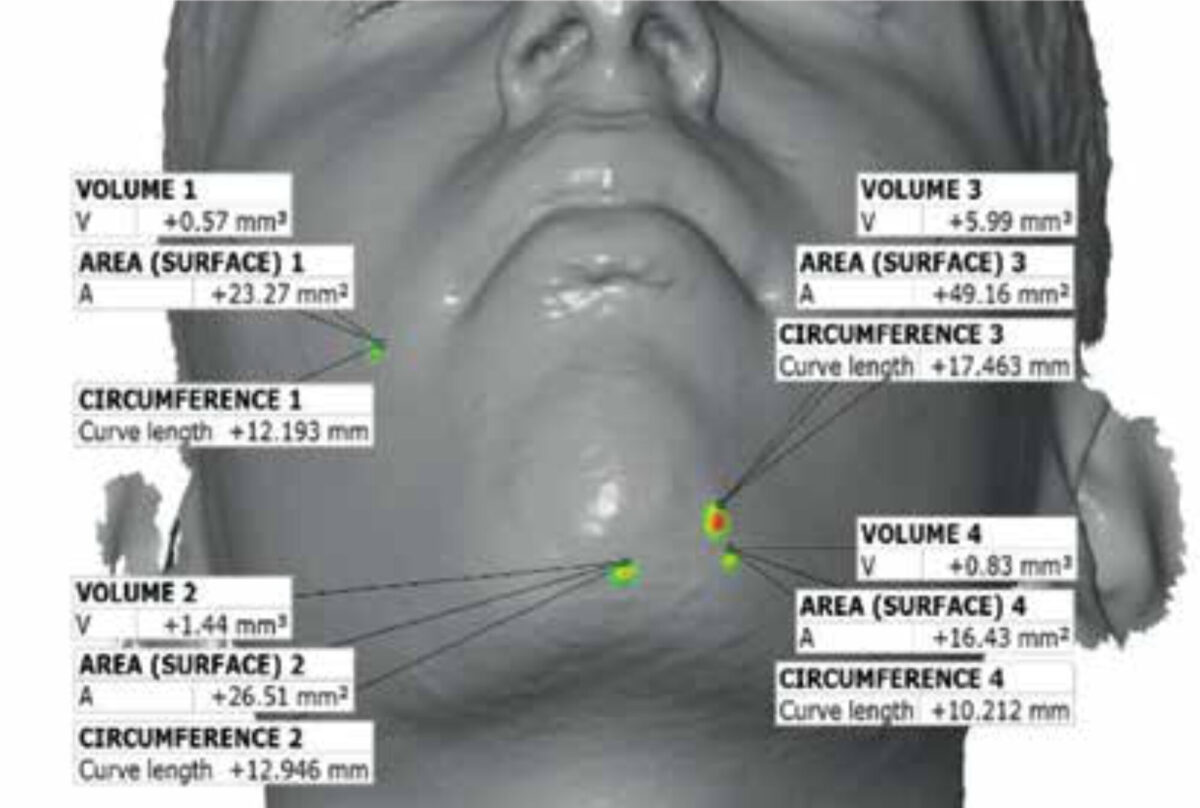
The scanning can be done by a mobile scanning device; only limited training is needed. The scan is imported into a laptop computer and with specific software a computerised image is constructed that allows measuring the circumference, surface, and volume of the lesion, including changes in skin colour. The latter is done by an engineer/technician and requires some more training.
This imaging modality is under investigation in tropical medicine. So far, it is being studied in mycetoma and post-kala-azar dermal leishmaniasis (PKDL), but this modality may be useful in other (infectious) conditions that affect the skin. Its main value may lie in the unrestricted, safe and inexpensive monitoring of these skin lesions in response to treatment as a biomarker, even under field conditions.
In mycetoma, the lesion is above and under the level of the skin, and an MRI scan is the gold standard. Obviously, an MRI scan requires a patient to travel to a central facility and has cost implications. Currently, research is ongoing to see if the lesion size above the level of the skin lesion may prove to be a proxy for the whole lesion, at diagnosis and during treatment (Figure 2). The 3D scan is therefore an ideal biomarker, as it can be done repeatedly, and it is safe; only patients who suffer from epileptic fits may be excluded as the flashes of light may trigger a seizure.
In PKDL Leishmania parasites persist in the skin after successful treatment of visceral leishmaniasis; the increasing immune response causes a maculo-papular or nodular rash surrounding the parasites. All lesions are above the skin surface, even the smallest lesions, can be measured. Subsequent computer images can be subtracted from one another making it possible to objectively record the difference between measurements with an accuracy of 0.1 mm (Figure 2, 3); this provides better accuracy than reporting via sequential (2-dimensional) photography, which is inevitably subjective.[10]

Conclusion
In summary, new applications of ultrasound imaging and innovative imaging tools such as 3D scanning are increasingly available and affordable for LMIC settings. Bedside diagnostics by the attending clinician saves time, helps to quickly narrow the differential diagnosis, and may be used in monitoring treatment. Integration in the medical curriculum should be considered also for those who are in training or who prepare to work in a resource-limited setting
References
- Nepal S, Dachsel M, Smallwood N. Point-of-care ultrasound rapidly and reliably diagnoses renal tract obstruction in patients admitted with acute kidney injury. Clin Med (Lond). 2020;20(6):541-4. doi: 10.7861/clined.2019-0417
- Assman NL, Kok B, Van Laarhoven A. Longechografie bij patiënten met symptomen van covid-19. Ned Tijdschr Geneesk. 2021;19:10-14
- Bélard S, Tamarozzi F, Bustinduy AL, et al. Point-of-care ultrasound assessment of tropical infectious diseases: a review of applications and perspectives. Am J Trop Med Hyg. 2016 Jan;94(1):8-21. doi: 10.4269/ajtmh.15-0421
- Limani F, Dula D, Keeley AJ, et al. Diagnostic point-of-care ultrasound in medical inpatients at Queen Elizabeth Central Hospital, Malawi: an observational study of practice and evaluation of implementation. Trans R Soc Trop Med Hyg. 2020 Nov 16;traa137. doi: 10.1093/trstmh/traa137. Online ahead of print
- Weber SF, Saravu K, Heller T, et al. Point-of-care ultrasound for extrapulmonary tuberculosis in India: a prospective cohort study in HIV-positive and HIV-negative presumptive tuberculosis patients. Am J Trop Med Hyg. 2018 Jan;98(1):266-73. doi: 10.4269/ajtmh.17-0486
- Phiri T, Zijlstra EE, editors. The clinical book. 3rd edition [in press]. Blantyre, College of Medicine, Department of Medicine
- Huson MAM, Kaminstein D, Kahn D, et al. Cardiac ultrasound in resource-limited settings (CURLS): towards a wider use of basic echo applications in Africa. Ultrasound J. 2019 Dec 27;11(1):34. doi: 10.1186/s13089-019-0149-0
- Treleaven P, Wells JCK. 3D body scanning and healthcare applications. Computer. 2007; 40(7):28-34. doi: 10.1109/MC.2007.2
- Liberton N, van Einatten M, te Slaa S, et al. 3-Dimensional scanning in a phase 2 trial in mycetoma in Sudan [poster]. Geneva: Geneva Health Forum; 2018
- Zijlstra EE, Liberton N, Musa AM, et al. Three-dimensional optical scanning in post-kala-azar dermal leishmaniasis (PKDL). Am J Trop Med Hyg. 2020 Feb;102(2):286-88. doi: 10.4269/ajth.19-0370


















































