Main content
In February 2020, the medical staff of the Congolaise Industrielle des Bois (CIB) hospital in Pokola, a small town in the department Sangha of the Republic of the Congo (Congo-Brazzaville), faced a small outbreak of monkeypox. All cases occurred in the same family of Mbendjele BaYaka, hunter-gatherers living in a small village in the rainforest of the Central Congo Basin, in the neigh-bouring department of Likouala (Figure 1).

Case description
In early February, the mother presented two children to the outpatient depart-ment of the hospital in Pokola. Patient A, a previously healthy seven-years-old boy, had a one-week history of fever, dry cough and a sore throat. He developed a rash two days after the start of the fever. Upon examination, a generalised vesicu-lar rash all over the body was seen, including palms of the hands and soles of the feet. Further of note was a gener-alised lymphadenopathy (Figure 2A, B).
His twenty-year-old sister, patient B, presented with a similar clinical picture that had started a few days later. However, pustules and crusts accompanied the vesicular rash, and the oral mucous membranes and the conjunctivae were affected (Figure 2C). On the sole of the right foot a deeper lesion was noted. Both patients did not appear ill and the fever on presenta-tion had subsided. The mother had no symptoms at all. Thorough history taking did not reveal a bite or scratch of animals, bush meat preparation, or other direct contact with dead animals. However, the mother mentioned that her son (patient A) might have eaten bush meat at another family house.
The third patient, patient C, the five-year-old sister of patient A and B, was admitted one week later with a history of fever for four days, a gener-alised vesicular rash for one day, loss of appetite and fatigue. On examina-tion, she appeared ill with a tempera-ture of 38°C and was dehydrated. The fourth and fifth case from the family, patients D and E, a sixteen-year-old girl and four-year-old boy respectively, turned up a few days later with the same clinical picture as the first two patients. They did not appear to be ill.
In view of the clinical picture and local epidemiology, the working diagnosis was monkeypox. Other diagnoses considered were chickenpox, scabies and pian (an endemic non-venereal trepo-nematosis). All of these were less likely, supported by the experience of an earlier smaller outbreak in 2019 with an identi-cal clinical picture that had occurred in the Likouala Department. The outbreak was confirmed as monkeypox virus infection by PCR techniques at the Laboratoire Nationale de Santé Public (LNSP) in Brazzaville with the help of the United States of America’s (USA) National Institutes of Health (NIH).

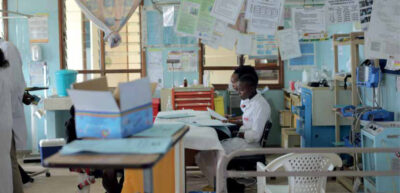
Case management in the hospital
After admission, all five patients were managed in a separate isolation ward following the Interim national guidelines for monkeypox outbreak response of the Nigerian Centre for Disease Control (NCDC) and the Nigerian Federal Ministry of Health.[1] After a refresher training on hygienic protocols and use of personal protective equipment (PPE), a team of nurses previously vaccinated against smallpox was designated to care for the patients. The patients were visited regularly for culturally appropri-ate psychosocial support by a Mbendjele BaYaka hospital guide. Strengthening nutrition was provided. Clinical man-agement consisted of daily assessment of the patients as well as providing supportive treatment in case of fever, aches and care of the skin lesions. All patients but one had an uncomplicated self-limiting course of the disease, and were discharged when the majority of the skin lesions had crusted (Figure 3). The remaining five-year-old girl, patient C, with dehydration and fever on admis-sion, went through an eventful course with vomiting, bloody diarrhoea, bouts of hypoglycaemia, pneumonia and respi-ratory distress. Despite intensive medi-cal treatment and nursing care, she died on the tenth day of admission. A safe and dignified burial was carried out.

Public health intervention in the district
The hospital staff organised an out-reach to the villages in the area where the disease originated. With the help of facilitators from an NGO expe-rienced in health communication with Mbendjele BaYaka, actions were explained to reduce animal-to-human and human-to-human transmission. With emphasis on the low fatality rate and self-limiting aspect of the disease, the aim was to reduce panic and stig-matisation. Previously trained and well installed Mbendjele BaYaka healers were instructed and provided with picto-grammed education material to ensure continued public health messaging.
Background on monkeypox
Monkeypox is a rare viral zoonotic disease, endemic to West and Central Africa. The causing virus belongs to the Orthopoxvirus genus that includes variola virus (the cause of smallpox), vaccinia virus (used in the smallpox vaccine), and cowpox virus. It was first discovered in 1958 when two out-breaks of a pox-like disease occurred in colonies of monkeys kept for research, hence the name ‘monkeypox’. Human cases were first reported in 1970 in the Democratic Republic of the Congo.[2] An outbreak in Nigeria, ongoing since 2017, is the largest documented.[3] Outside of Africa, from 2003 to date, cases of human monkeypox infections have been documented in four countries: United Kingdom, Israel, Singapore and the USA.[4] These imported cases have all been associated with travel from Nigeria.
The animal reservoir of monkeypox remains unknown. Evidence suggests that it may be rodents and squirrels. Transmission through direct or indirect contact with animals – live or dead animals – including through bush meat consumption, hunting, or trade, is presumed to be the main factor for human monkeypox infections. Human-to-human transmission is less common but possible through close contact with an infected person’s skin lesions and large respiratory droplets exhaled during extended face-to-face contact. The incu-bation period averages between seven to fourteen days. The symptoms, which are usually self-limiting, begin with fever, lymphadenopathy, and myalgia, within a few days followed by skin eruptions, all over the body, with mucous mem-branes also affected. The rash develops sequentially from macules to papules to vesicles and finally to pustules which crust, dry and fall off. Lymphadenopathy is a key feature that can help to differ-entiate monkeypox from diseases with similar initial presentation (e.g. chick-enpox, measles, smallpox). Case fatality rates range from 1% to 11%, highest with the Central African viral clade and younger children. No specific treat-ments are available. No vaccine is cur-rently licensed. Observational trials have shown that smallpox vaccines provide up to 85% protection against monkey-pox. PCR testing of skin lesion swab or urine sample, and sequencing confirm the diagnosis of monkeypox infection.
Sudden outbreaks with a potentially high transmission risk, such as the one described here, need to be counteracted by public health measures such as case detection, case isolation, appropriate community health messaging and pro-tective measures for health care workers.
Conclusion
Monkeypox is a rare viral disease with a low case fatality rate. Increased human-animal interactions are likely to cause (larger) outbreaks in the future. With knowledge of local epidemiology and good clinical reasoning, it can be diagnosed, even if sophisticated labora-tory support is not at hand. Protocols from national disease control centres such as the NCDC as well as online local and international consultation are recommended for proper manage-ment and public health interventions.
Acknowledgements
We thank Dr. Jean Vivien Mombouli, Dr. Cynthia Nkoua (LNSP), Dr. Vincent Munster and Dr. Robert S. Fisher (NIH) for the analysis of the monkey-pox samples of the outbreak of 2019. We thank Project Bwanga for support with our public health messaging.
References
- Federal Ministry of Health, Nigerian Centre for Disease Control. Interim National Guidelines for Monkeypox Outbreak Response [Internet]. Jab Abuja: Federal Ministry of Health, Nigerian Centre for Disease Control; 2017 Oct [accessed 2021 Aug 22]. 48 p. Available from: https://ncdc.gov.ng/themes/common/docs/protocols/50_1508912430.pdf.
- CDC [Internet]. Atlanta: Centers for Disease Control and Prevention; 2021. Monkeypox; 2021 Jul 21. Available from: https://www.cdc.gov./poxvirus/monkeypox/
- Yinka-Ogunleye A, Aruna O, Dalhat M, et al. Outbreak of human monkeypox in Nigeria in 2017-18: a clinical and epidemiological report. Lancet Infect Dis. 2019 Aug;19(8):872-9. doi: 10.1016/S1473-3099(19)30294-4. Epub 2019 Jul 5
- WHO [Internet]. Geneva: World Health Organization; organization; 2021. Monkeypox; assessed 2021 Aug 22. Available from: https://www.who.int/emergencies/emergency-events/item/monkeypox