Main content
Setting
The Lion Heart medical centre is located in Yele, a small town in the middle of Sierra Leone. This new rural hospital opened in 2012 and has a capacity of 32 beds divided in a male, female, pediatric and maternity ward. The medical staff consist of one medical officer, two clinical health officers and qualified local nurses. The hospital has a surgery room, basic laboratory facilities and digital radiography equipment. The nearest specialist hospitals are six hours away by car.
Case report
A sixty-five year old woman presented at the outpatient ward with complaints of a persisting wound on the heel of the right foot. The lesion occurred spontaneously one year ago; there had been no trauma. Recently the wound started to ulcerate and she developed a fever. No evacuation of pus was observed.
No relevant medical history or medication use was noted. The wound was painful and while walking the patient put her weight on the forefoot.
On examination she appeared healthy, there was no fever. On the plantar-medial side of the right heel there was a lesion with an irregular shape but with well-defined margins; it was depigmented, erosive and measured approximately ten by ten centimeters. In the centre a couple of irregular well-defined pigmented maculae were present with different stages of hyperpigmentation (Figure 1). There was no ulceration and no pus. Bilateral small inguinal lymph nodes were palpable. The hemoglobin was 8.5 g/dL and a malaria test was negative. An X-ray showed normal bone structures of the calcaneus and other parts of the ankle joint.
A malignant disease was suspected for which biopsy was needed for confirmation. Pathology services in Sierra Leone take a long time and are unreliable. Consult Online was asked for advice concerning the differential diagnosis and diagnostic and treatment options. With a suspicion of a malignant disease the local doctor proposed local excision or amputation.


Advice from the specialists
Three dermatologists replied within 5 hours. They all agreed with the local doctor; malignancy was probable but a biopsy would be needed to confirm the diagnosis. The most probable diagnosis was an acral lentiginous melanoma. The dermatologists proposed a wide local excision. If the excision area did not heal, amputation could be performed in a later stage. The excised tissue should be sent to the Netherlands for histological examination.
Acral lentiginous melanoma
Acral lentiginous melanoma is a subtype of the cutaneous melanoma occurring on the hands and feet. Although the acral lentiginous melanoma is rare in Caucasians, it is the most common subtype of melanoma in populations with darker skins. It is most often seen on the soles of the feet, but also occurs on the palms and subungual regions. 1-2 About half of the hand and feet melanomas concern the acral lentiginous melanoma subtype. 2
There are limited research data about early diagnosis and treatment of this specific subtype of melanoma. Acral naevi and trauma have been identified as possible risk factors, whereas UV-radiation seems to play little or no role at all. Prognosis of the acral lentiginous melanoma is poor in comparison to other melanomas, most probably because of the late diagnosis. It is also possible that this type of melanoma is more aggressive thus leading to a poor prognosis. The most important prognostic factors are the depth of the lesion according to the Breslow thickness scale and the presence of ulceration. This is comparable to the other cutaneous melanomas, although the prognostic factors seem to be less reliable to predict the outcome. 2
Treatment
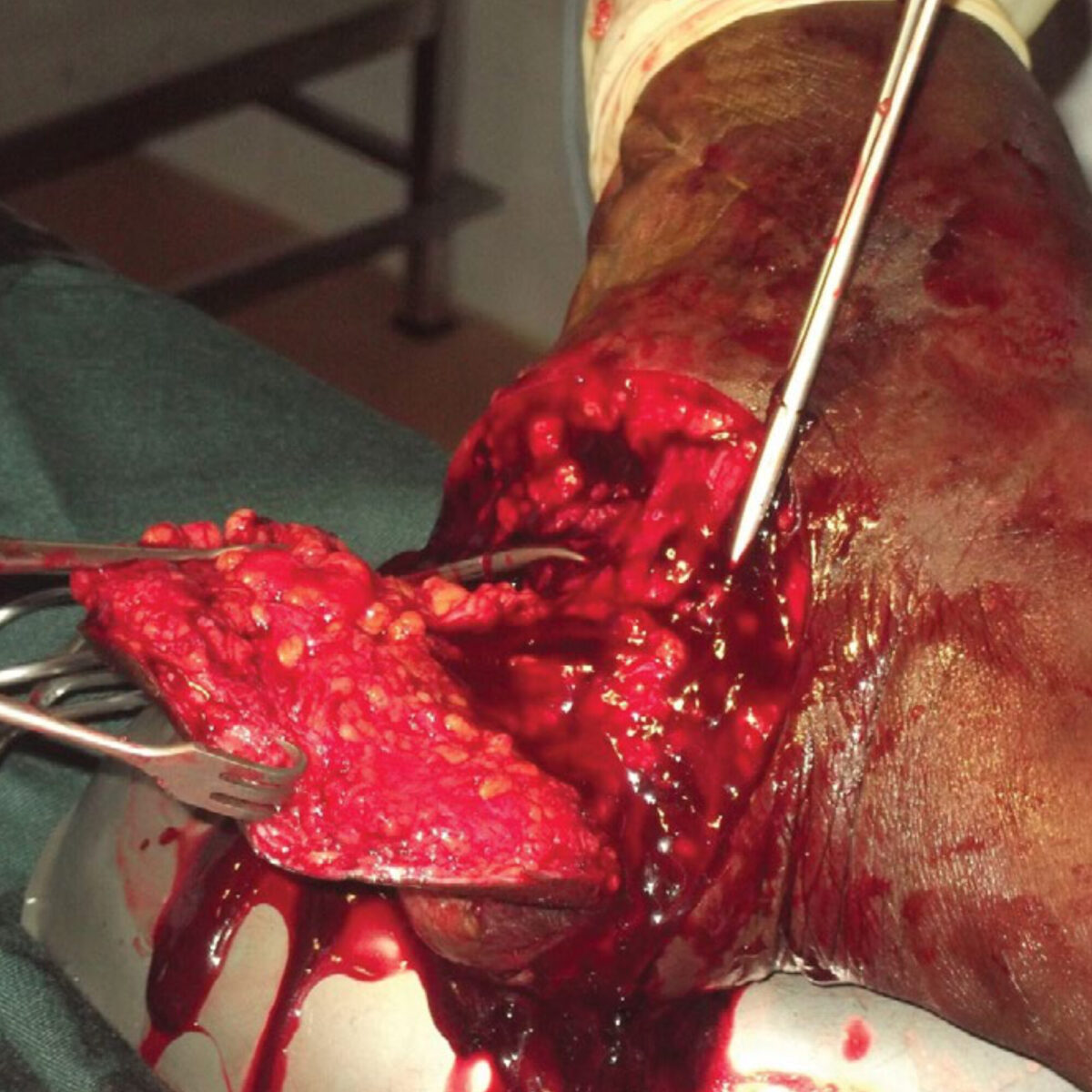
Wide local excision was performed after consent of the patient and family. Macroscopically no signs of local growth were visible. After one week the wound of the excision area was granulating well and a skin graft was planned shortly. (Figure 2 and 3)
Follow-up
After 6 weeks the pathology report from the Netherlands showed an unclassified malignant melanoma with a Breslow thickness of 5 mm. The excision margins were not free of melanoma cells. With this Breslow thickness and the incomplete excision of the melanoma the prognosis was expected to be poor. The specialists hoped the excision would be sufficient but believed metastasis in the regional lymph nodes and/or hematogenous metastasis was likely. Because of the (local) therapeutic restraints the advice was to provide optimal palliative care when clinical suspicions for metastasis would arise.
References
- Kundu RV, Patterson S. Dermatologic conditions in skin of color: part I. Special considerations for common skin disorders. Am Fam Physician. 2013 Jun 15;87(12):850-6.
- Durbec F, Martin L, Derancourt C, Grange F. Melanoma of the hand and foot: epidemiological, prognostic and genetic features. A systematic review. Br J Dermatol. 2012 Apr;166(4):727-39.


















































