Main content
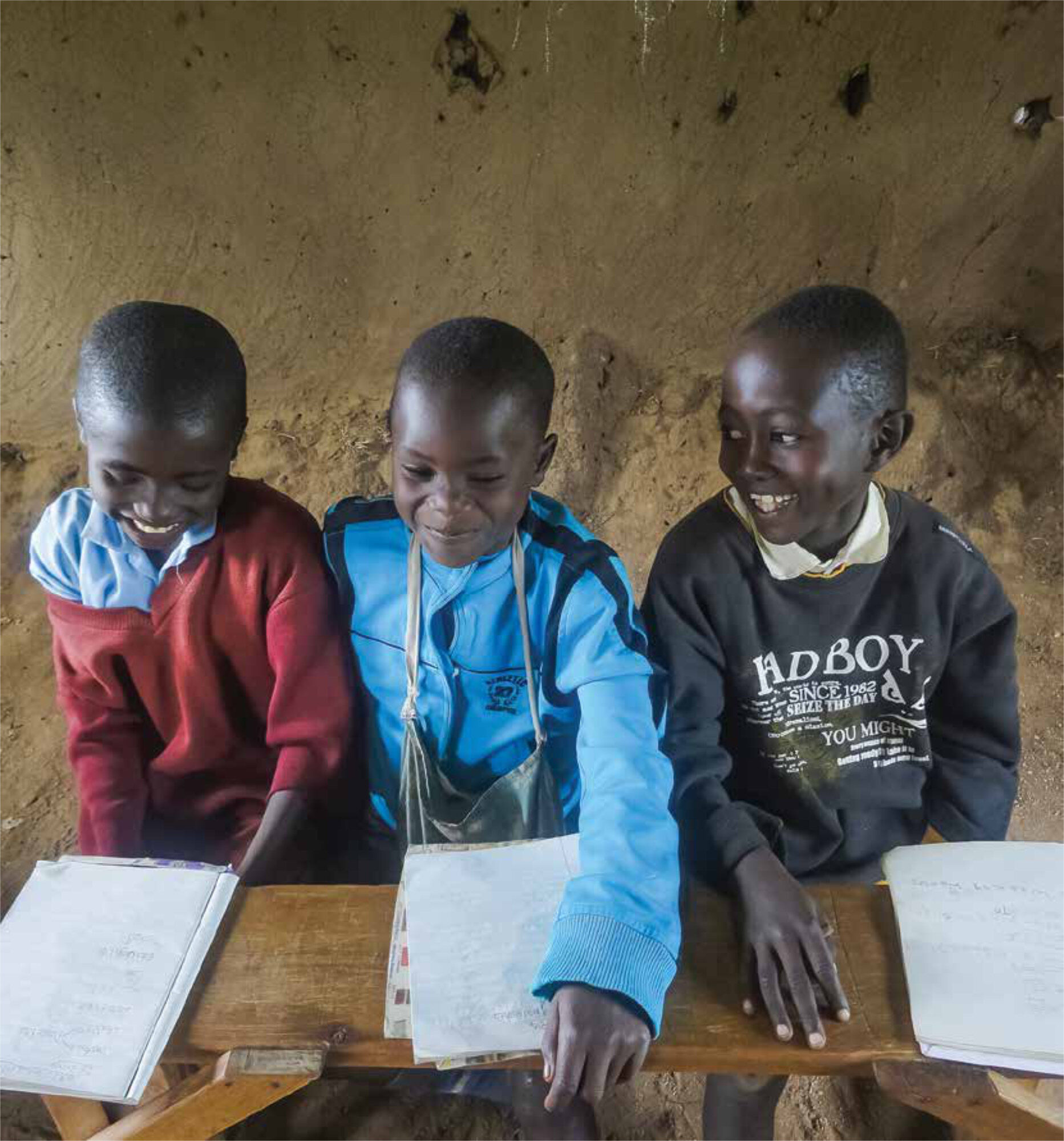
In developing countries, the prevalence of anaemia is high in children. In large parts of Africa, two out of three children are anaemic (defined by a haemoglobin [Hb] of <11 mg/dl or 6.6 mmol/L). A relatively small percentage (< 5%) of these children are severely anaemic (Hb < 5 mg/dl or 3.0 mmol/L). The mortality due to severe anaemia can be up to 18%, and severe anaemia is therefore, in many regions, a major contributor to the high Under-5-Mortality-Rate.
Childhood anaemia in resource poor settings
With an estimated prevalence of 57%, pregnant women are another important high-risk group for anaemia in these regions. Anaemia during pregnancy negatively influences growth and development of the foetus and increases the risk of complications during labour. Despite the multifactorial aetiology of anaemia in resource poor settings, treatment programs are still mainly focused on iron supplementation, despite its possible harmful effects. A shift of focus in the treatment of (childhood) anaemia in these settings is needed.
Aetiology and pathophysiology of anaemia
Since iron is essential for synthesis of haemoglobin, iron deficiency is often considered the primary cause of anaemia. The terms anaemia, iron deficiency and iron deficiency anaemia are often interchanged, although they mean different things. Besides being confusing in terms of definitions, this ignores the fact that anaemia can occur even with sufficient iron stores. And iron deficiency does not necessarily lead to anaemia, as in the initial stages of iron deficiency, erythropoiesis is not restricted.
Recent studies have shown that the aetiology of anaemia is complex and that multiple factors, through different pathophysiological pathways, may lead to anaemia. Blood loss, haemolysis and decreased erythropoiesis are the three mechanisms leading to (severe) anaemia, each of them having its own set of aetiological factors (Table 1). It is important to note that the contribution of the various aetiological factors varies by region and population. For example, infections such as hookworm and schistosomiasis are frequently found in children living in rural areas (prevalence may be above 20%), but are rarely found in children living in urban settings (prevalence often below 2%). It is noteworthy that hookworm may cause serious infection already at a very young age (< 1 year).² Another example of a cause of anaemia that varies by region is vitamin B12 deficiency. In Cameroon, prevalence varied between 11% and 30%, whereas in Malawian children, the prevalence of vitamin B12 deficiency did not vary by region but was correlated with the severity of anaemia (15% in moderate anaemic and 30% in severely anaemic children.¹ Iron deficiency was found to play a role in the development of mild and moderate anaemia, but no association was identified between iron deficiency and severe anaemia in a Malawian study.
Besides the geographic diversity of factors causing anaemia, the individual factors may interact or correlate. For example, it has recently been shown that the association between vitamin A and severe anaemia could in part be explained by the effect of vitamin A deficiency on susceptibility to malaria and bacterial infection. In addition, HIV can be a direct cause of anaemia by infecting bone marrow stem cells, which causes apoptosis of these cells and thereby affects the red cell production capacity. Yet HIV may, due to its immune-suppressive effect, also increase the susceptibility to infections and thereby the risk of anaemia via suppression of the bone marrow through a non-specific inflammatory response.³
Treatment and prevention of anaemia
With respect to the role of iron in the treatment of anaemia, it is important to note that over the past decades there has been an on-going debate on the complex interaction between iron deficiency, iron supplementation, and susceptibility to infections. Iron deficiency may increase risks of infection, as iron is required for normal immune function, including bactericidal activity of macrophages and T-cell function.⁴
However, on the other hand, since iron is also an essential nutrient for many pathogens, iron deficiency may protect the host against infections. This was demonstrated by studies indicating that iron deficiency is associated with a reduced risk of malaria infection.⁵,⁶ This so-called protective functional iron deficiency is largely mediated by hepcidin.⁷,⁸
In 2006, a large trial in Zanzibar found that iron was associated with an increase in morbidity and mortality in iron supplemented children.⁹ More recent studies have found a strong positive relationship between iron supplementation and susceptibility to malaria.¹⁰ As a result, the World Health Organization has decided to restrict its recommendations for iron supplementation to children with severe anaemia or proven iron deficiency. The problem is, however, that iron status is difficult to assess due to lack of available iron markers which are not influenced by the acute phase response occurring during an infection.¹¹ Furthermore, in severely anaemic children, hepcidin levels were found to be low, despite concurrent severe infections, thereby possibly missing the protective effect of inhibited iron absorption in the gut (which would be the response to a high hepcidin level) and increased infection risk.¹² Besides the above mechanism, the harmful effects of iron supplementation are likely to be context-specific, because exposure to pathogens and thereby the risk of infection differs by area.⁵,⁶,⁷
Folic acid deficiency is also generally regarded as a potential cause of anaemia in children. However, few studies have measured folic acid levels in children living in developing countries. Studies in Gambia and Malawi detected very few children who were folic acid deficient and found no beneficial effect of folic acid supplementation on haemoglobin recovery.¹³ In addition, one has to take into account that folic acid supplementation, if not indicated, may not be a harmless treatment. Folic acid may stimulate the growth of Plasmodium falciparum and inhibit the effectiveness of the antimalarial drug sulphadoxine-pyrimethamine (SP).
Although vitamin A deficiency is an important cause of anaemia, supplementation had surprisingly little effect on the incidence of severe anaemia in children, which might indicate that other concurrent conditions had caused the anaemia.
| Mechanism | Etiological factors | |
|---|---|---|
| Blood loss | Through urine, stool or trauma | Hookworm Schistosomiasis Shigellosis Traffic accident, crocodile or hippo bite |
| Haemolysis | Intra- or extra-vascular | Malaria Sepsis Haemoglobinopathies (SCD, Thalassemia, G6PD) |
| Decreased erythropoiesis | Bone marrow failure through infections | Parasitic: Malaria Bacterial: Tuberculosis, ‘Non-typhoid Salmonella’ Viral: HIV, Parvovirus, EBV, CMV |
| Micronutrient deficiencies | Deficiency of Iron, folic acid, vitamin B12, vitamin A | |
Conclusions
Management of (severe) anaemia must be underpinned by a detailed knowledge of the multifactorial aetiology which varies geographically, seasonally and between sub-populations. Therefore, anaemia is unlikely to be amenable to a single intervention, and global strategies are usually not applicable. It is increasingly clear that restoring the function of the bone marrow is essential in the treatment of anaemia. However, multiple bone marrow suppressive factors are often at play simultaneously. All these factors need to be addressed, as otherwise the bone marrow will remain blocked. More research and strong partnerships between programmes are needed to determine appropriate intervention packages that are tailored to the local causes of anaemia.
GLOBAL CHILD HEALTH GROUP, EMMA CHILDREN’S HOSPITAL AND DEPARTMENT OF GLOBAL HEALTH, ACADEMIC MEDICAL CENTRE, UNIVERSITY OF AMSTERDAM.
References
- Calis JC, Phiri KS, Faragher EB, et al. Severe anemia in Malawian children. N Engl J Med 2008 Feb 28;358(9):888-99.
- Nkhoma E, Boele van Hensbroek P, van Lieshout L, Boele van Hensbroek M. Severe anaemia in an 11-month-old girl. Lancet 2005 Mar 26;365(9465):1202.
- Calis JC, Phiri KS, Vet RJ, et al. Erythropoiesis in HIV-infected and uninfected Malawian children with severe anemia. AIDS 2010 Nov 27;24(18):2883-7.
- Beard JL. Iron biology in immune function, muscle metabolism and neuronal functioning. J Nutr 2001 Feb;131(2S-2):568S-79S.
- Gwamaka M, Kurtis JD, Sorensen BE, et al. Iron Deficiency Protects Against Severe Plasmodium falciparum Malaria and Death in Young Children. Clin Infect Dis 2012 Apr;54(8):1137-44.
- Jonker FA, Calis JC, Boele van Hensbroek M, et al. Iron status predicts malaria risk in Malawian preschool children. PLoS One 2012;7(8):e42670.
- Kroot JJ, Tjalsma H, Fleming RE, Swinkels DW. Hepcidin in human iron disorders: diagnostic implications. Clin Chem 2011 Dec;57(12):1650-69.
- Cassat JE, Skaar EP. Iron in infection and immunity. Cell Host Microbe 2013 May 15;13(5):509-19.
- Sazawal S, Black RE, Ramsan M, et al. Effects of routine prophylactic supplementation with iron and folic acid on admission to hospital and mortality in preschool children in a high malaria transmission setting: community-based, randomised, placebo-controlled trial. Lancet 2006 Jan 14:367(9505):133-43.
- Esan MO, Boele van Hensbroek M, Nkhoma E, et al. Iron supplementation in HIV-infected Malawian children with anemia: a double-blind, randomized, controlled trial. Clin Infect Dis 2013 Dec;57(11):1626-34.
- Jonker FA, Boele van Hensbroek M, Leenstra T, et al. Conventional and novel peripheral blood iron markers compared against bone marrow in Malawian children. J Clin Pathol 2014 Aug;67(8):717-23.
- Jonker FA, Calis JC, Phiri K, et al. Low hepcidin levels in severely anemic malawian children with high incidence of infectious diseases and bone marrow iron deficiency. PLoS One 2013;8(12):e78964.
- Boele van Hensbroek M, Morris-Jones S, Meisner S, et al. Iron, but not folic acid, combined with effective antimalarial therapy promotes haematological recovery in African children after acute falciparum malaria. Trans R Soc Trop Med Hyg 1995 Nov;89(6):672-6.