Main content
Results from data collection in the Hawassa university referral hospital Ethiopia
Injuries account for 10% of deaths worldwide. This is higher than the total number of deaths from malaria, tuberculosis and HIV combined. Road traffic accidents are responsible for 23% of these, followed by intentional harm from suicide (15%) and homicide (11%). Low- and middle-income countries (LMICs) suffer the brunt of these, with injury death rates ranging from 45-55 fatal injuries per 100,000 population in Western Europe and North America up to 99 to 126 in LMICs. [1] These numbers are rising in sub-Saharan Africa due to rapid growth of motorized transport and expansion of industrial production without adequate safety precautions. [2] Only little attention is given to this problem and thus there is insufficient monitoring of the pattern and burden of injuries. In 2012, 11% of the total disability adjusted life years (DALYs) lost in Ethiopia were due to trauma. [3] Our aim is to describe the causes and type of injuries in Hawassa University Referral Hospital in 2013 (2006 Ethiopian calendar) and to make recommendations for possible interventions.
Experiences from an ethiopian hospital
We performed a retrospective cohort study in Hawassa University Referral Hospital in Ethiopia. All trauma patients who presented in either the surgical or the paediatric emergency department (ED) in 2013 were included. We collected their file numbers from the logbooks in the emergency and paediatric department. Using a structured checklist, socio-demographic and injury-related facts were recorded. In case of multiple injuries but no poly trauma, we selected the most severe injury.
The hospital
Hawassa University Referral Hospital is a large tertiary hospital (79 surgical beds, 8 intensive care beds) for the southern region of Ethiopia that serves a population of 19.1 million people. At the time of research, there were eight general surgeons, one of them also specialized in urology and one in plastic and reconstructive surgery. None were formally trained as trauma or orthopaedic surgeon. The hospital serves as a training facility for medical students and provides postgraduate training for surgical residents and emergency physicians. Residents or emergency physicians are usually the first responder in the ED. No structured triage system is in place and trauma cases are not structurally assessed via Advanced Trauma Life Support (ATLS) principles. X-ray and ultrasound possibilities are available. No CT scan was available at the time. Those who could afford it were sent to a private hospital with CT facilities. We should mention here that, contrary to the situation in most high-income countries, there is a possibility of keeping patients in the ED for several days, and these patients did not count as admissions.
Results
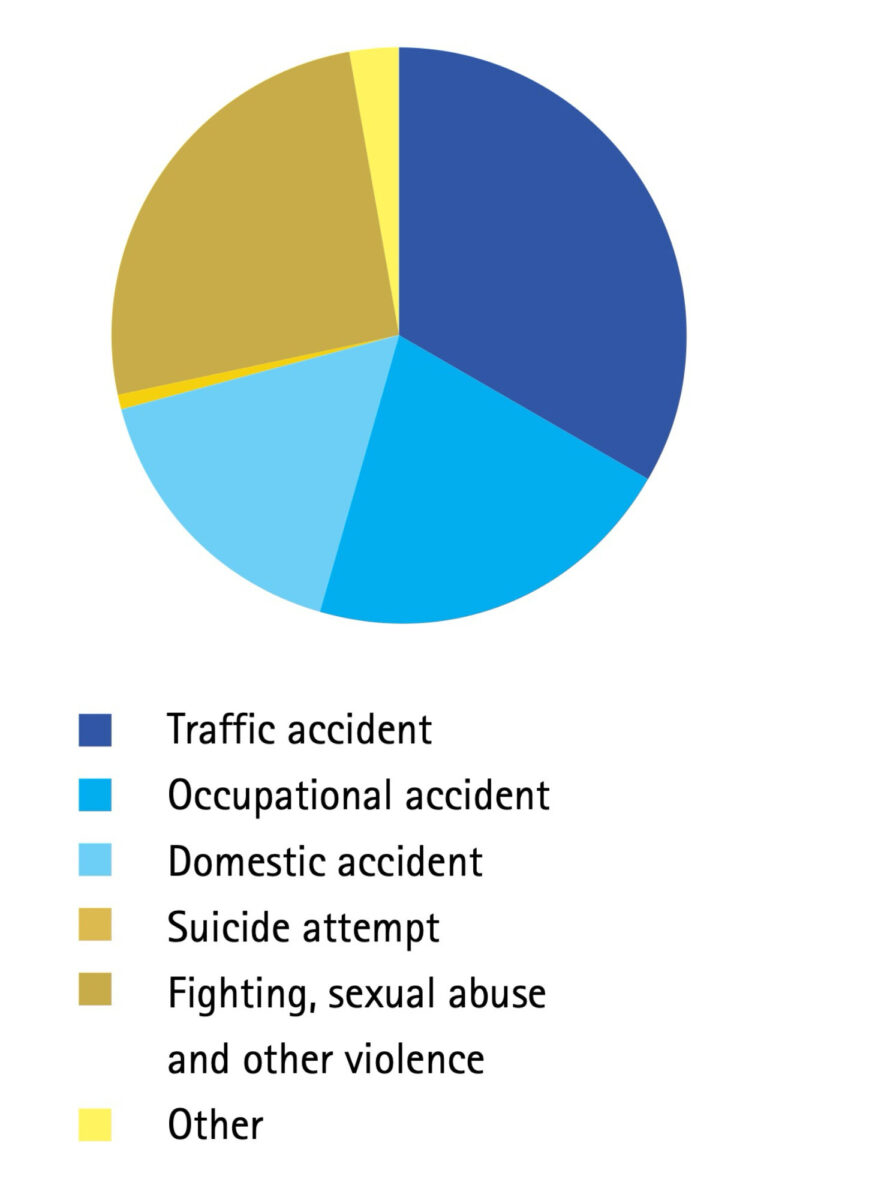
In 2013, in total 1318 patients presented with trauma in either the emergency or paediatric department of our hospital. We excluded 14 patients from our study due to missing files. Finally, 1304 patients were included, of which 30% were referred by a lower-level facility. Two-thirds were male, median age was 28 years (ranging from 0 to 90 years). Unintentional harm accounted for 70% of the injuries: mainly road traffic accidents (36%), occupational accidents (19%) and domestic accidents (15%). Fighting, sexual abuse and other intentional harm accounted for 28% of the cases, while suicide attempts were seen in less than 1%. The remaining cases were mostly from animal attacks (e.g. hyena-, dog- and snakebites). See also Figure 1.
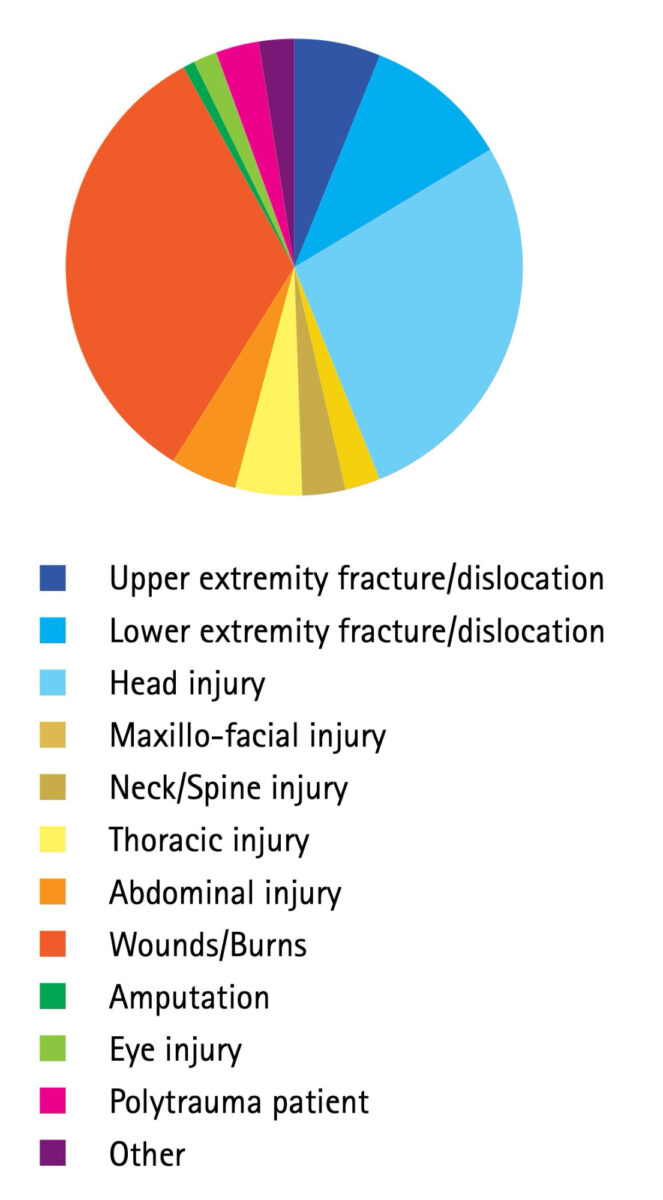
In terms of injury types, the most frequent were wounds and burns (N=395, 36%), although most of these cases were only mild (85%). Second most frequent were head injuries (N=381, 29%). Of these, severe head injuries were seen in 21% of the cases, 22% had moderate head injuries and 57% only mild head injuries. Only 2% of the patients were poly trauma patients. Location of injury is provided in Figure 2.
Head trauma was a major reason for presentation at the ED. Half of these (187) needed admission. From this group, 29 needed burr holes. A total of 45 head injury patients died during admission. This was the leading cause with 66% out of the total in-hospital deaths after trauma.
Because of a lack of orthopaedic surgeons, 57 patients (4.4%) were referred to another hospital. Almost half of those patients (24/57) were sent for orthopaedic treatment of lower or upper extremity fractures or dislocations, 14 were referred because of head injuries, 6 because of complicated poly trauma, and 12 for the treatment of other injuries.
Discussion
We described the causes and types of injuries in a large tertiary hospital in Ethiopia during one year. Unfortunately, little epidemiological data is available on injuries in Ethiopia. [4,5] We believe that more data would be crucial for health policy makers to guide their decisions on in-hospital care as well as on preventive measurements. Compared to recently published data collected elsewhere in Ethiopia, we found similar rates of road traffic accident victims: 34% in our study, 35% in Bulto et al. versus 14% in Amdeslasie et al. [4,5] We found slightly less victims from intentional harm (28%) than Bulto et al (43%) and Amdeslasie et al (31%). Mainly young men are affected. Most common are soft tissue and head injuries, with the latter type accounting for both most admissions and in-hospital deaths. We found an in-hospital mortality of 5.4%, mainly after head injury. This is comparable to the 4.2% in a recent study about trauma in a tertiary hospital in Malawi. [6] Head injury accounted for most of our admissions, similar to the studies by Bulto et al and Amdeslasie et al. [4,5]
We hypothesize that we underestimated the true trauma related morbidity and mortality. Firstly, not all patients reach the hospital alive. There are no comprehensive statistics about victims who died on the accident scene or while being transported to the hospital. Another category that do not make it to our tertiary referral hospital are those that are seen in a local clinic but cannot afford the travel costs. Thirdly, we only looked at admissions. Patients seen and treated in the ED, even if for an overnight observation there, were not included. Another limitation is the retrospective nature of this study. The coding system used in this study was not standardized in the hospital admission forms. This means that the files had to be reviewed and interpreted by the researchers, sometimes with incomplete data. The earlier mentioned lack of trauma skilled personal was confirmed by the lack of structured trauma screening found in this retrospective study.
Our data cannot directly be extrapolated to other low-resource settings but gives a mere indication of the trauma burden in a referral hospital in an Ethiopian rural area.
Multilevel interventions are needed to diminish the high burden of trauma victims in southern Ethiopia, including a focus on preventive care
Recommendations
As we consider the burden of injuries to be high, we propose that multilevel interventions are needed to diminish the high burden of trauma victims in southern Ethiopia, including a focus on preventive care.
In the first place, the hospital staff is not trained in trauma care and resources are limited. Although there is no formal training available in Ethiopia, we recommend inclusion of the principles of ATLS during medical and postgraduate training. [7] Also, the scarce availability of diagnostics that are essential in trauma care such as ultrasound and CT should be improved and made readily available. Furthermore, the limited treatment options, especially for traumatic bone injuries, play a major role in the outcome of trauma care. Often conservative treatment via plaster of Paris (POP) or skin or bone traction for fractures are the sole options available. The option of plating or intramedullary fixation is absent and there is only limited availability for external fixation, even in a tertiary referral centre. Inadequately treated fractures in young patients may lead to disability, more DALYs and hence less productivity for Ethiopia as a whole. Some (mission) hospitals provide orthopaedic care via expatriate trauma/ orthopaedic surgeons. However, there is a lack of trained Ethiopian trauma surgeons, especially in remote areas.
Secondly, prevention of trauma remains key. This prevention should primarily focus on traffic safety by addressing poor road structure, poor adherence to traffic rules, and the use of poorly maintained motorized vehicles and lack of use of safety equipment like helmets. Also, substance abuse (qat, alcohol) should be strictly controlled especially in traffic. Burns by cooking fires at home or kerosene lights pose a significant risk in relation to the high burden of burns we have encountered (36%). Occupational incidents could be prevented by better regulation of personal protective equipment at work.
Conclusion
In 2013, 1304 trauma patients were admitted after being seen in the emergency and paediatric department of Hawassa University Referral Hospital, most often due to road traffic accidents. Traumatic brain injury was the predominant reason for admission and for in-hospital death. Improvements could be made in the training of medical staff with the principles of ATLS or the presentation of multiple casualties. Policy makers should focus on enhancing the in-hospital trauma care and the referral system but above all should invest in preventive measures.
Co-authors
TOM GRESNIGT, MD
Department of Surgery, Hawassa University Referral Hospital, Hawassa, Ethiopia.
Department of Surgery, Treant Scheper Hospital, Emmen, the Netherlands.
tgresnigt@hotmail.com
W.W.E. NOLET, MD
Masanga Hospital, Sierra Leone.
D. VAN DER VELDE, MD, PHD
Department of Surgery, Hawassa University Referral Hospital, Hawassa, Ethiopia.
Department of Surgery, Trauma Unit, St Antonius Hospital, Nieuwegein, the Netherlands.
N. VAN DER NAALD, MD
Department of Surgery, Trauma Unit, St Antonius Hospital, Nieuwegein, the Netherlands
References
- WHO. Injuries and violence: the facts. https://www.who.int/violence_injury_prevention/key_facts/en [accessed on January 6th, 2019].
- Nordberg E. Injuries as a public health problem in sub-Saharan Africa: epidemiology and prospects for control. East Afr Med J. Kenya; 2000 Dec;77(12 Suppl):S1-43.
- WHO. Global Health Observatory data re-pository. Estimates by country: Age-standard-ized DALY rates Data by country. 2012
- Bulto LN, Dessie Y, Geda B. Magnitude, causes and characteristics of trauma victims visiting Emergency and Surgical Units of Dilchora Hospital, Eastern Ethiopia. Pan Afr Med J. Uganda; 2018;30:177.
- Amdeslasie F, Kidanu M, Lerebo W, Ali D. Patterns of trauma in patients seen at the emergency clinics of public hospitals in Mekelle, Northern Ethiopia. Ethiop Med J. Ethiopia; 2016 Apr;54(2):63-8.
- Tyson AF, Varela C, Cairns BA, Charles AG. Hospital mortality following trauma: an analysis of a hospital-based injury surveillance registry in sub-Saharan Africa. J Surg Educ. United States; 2015;72(4):e66-72.
- Tumwesigye NM, Ingham R, Holmes D. Condom use at first and latest sexual events among young people: Evidence from a rural and peri-urban setting in Uganda. Afr Health Sci. 2013;13(2):407-14.



















































