Main content
What useful contribution can Dutch researchers make to tropical medicine and international health? In recent years an increasing role is being played by researchers from low- and middle-income countries (LMIC), while research funding in many industrialized countries is being reduced. Yet, the research infrastructure is most developed in industrialized countries and human and financial resources in low- and middle-income countries are still limited. The most successful field research in tropical medicine and international health is the result of international collaboration between research institutes in low- and middle-income countries and industrialized countries. Technological developments (new diagnostics, drugs, vaccines) mainly arise in industrialized countries, although an increasing role of emerging economies is taking shape. Field trials take place primarily in high burden countries. Tuberculosis (TB) is used as an example to demonstrate these developments.
Ending neglect
In the 1970s and 1980s TB control had reached a stage of neglect in industrialized countries based on the wrong assumption that lasting control had been achieved [1]. From 1990 TB control and research received increasing attention and funding through a combination of factors. In New York a large outbreak of TB was brought under control with difficulty [2]. The first Global Burden of Disease study showed that, worldwide, TB was in the top ten causes of mortality [3]. The World Bank released a report in 1993 showing that TB control through diagnosis and treatment was among the most cost-effective interventions [4]. The impact of the HIV epidemic on TB incidence in Africa was tremendous [5], and the emergence of multidrug resistant, followed by extensively resistant TB was considered a major threat [6]. More recently, the impact of the Global Stop TB Strategy was shown to lag far behind the projections, despite great progress in coverage and treatment success [7]. While over the past two decades many tuberculosis deaths have been averted, the ‘treatment as prevention’ approach of tuberculosis control with currently available tools is clearly not sufficient to achieve tuberculosis elimination in the foreseeable future.
Research and development
Over the past two decades, major progress has been made in tuberculosis research as well. The genome of M. tuberculosis has been deciphered [8], bringing tuberculosis biology research back into mainline biological research, and providing an additional basis for the development of new diagnostics, drugs, and vaccines. Moreover, molecular markers were identified, leading to major progress in the molecular epidemiology of tuberculosis [9].
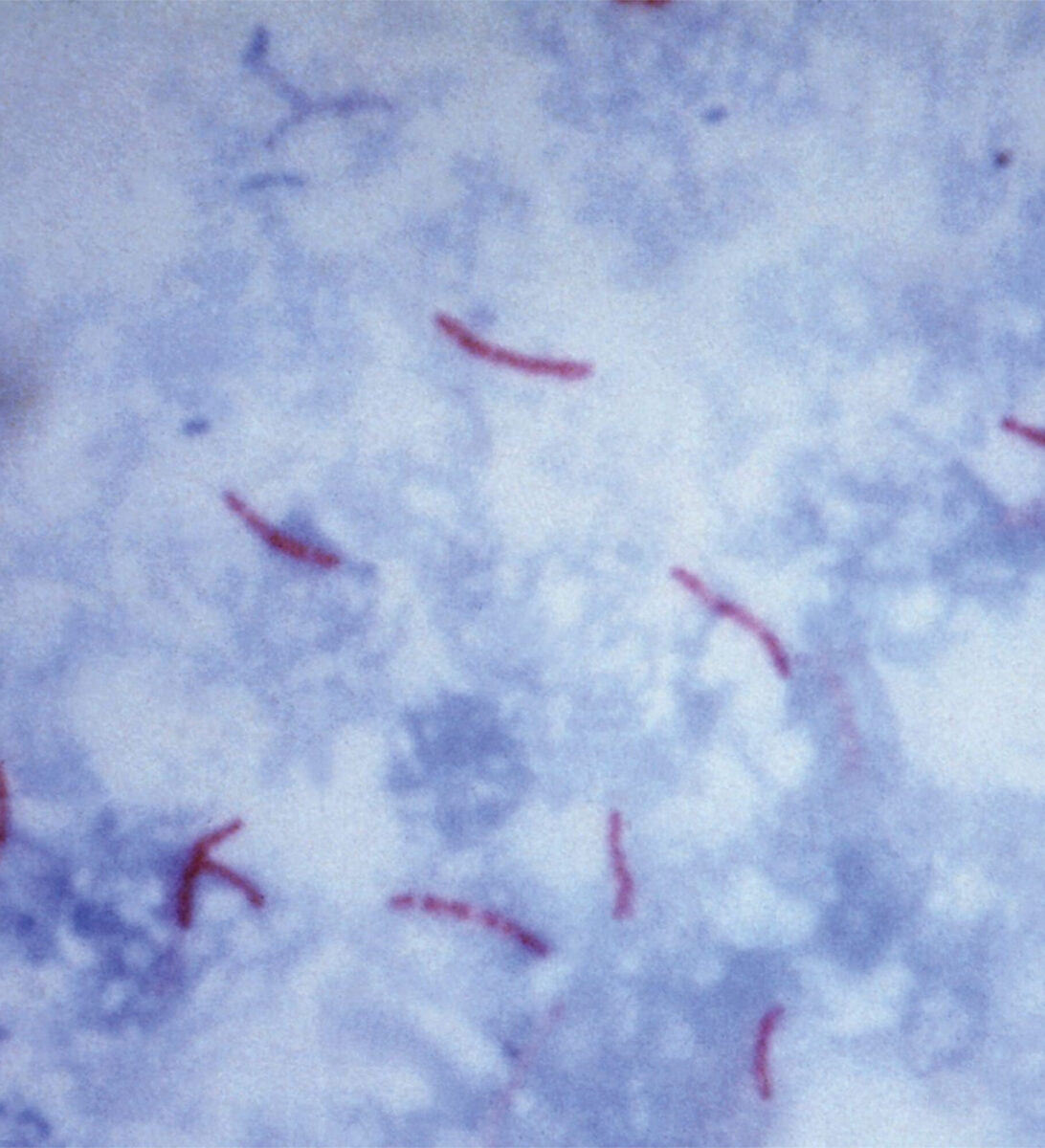
The diagnosis of tuberculosis relies heavily on sputum smear microscopy which has limited sensitivity, and culture, which is technically demanding and slow. The recent introduction of GeneXpert is a major step forward, allowing more sensitive and faster TB diagnosis, as well as rapidly identifying drug resistance [10]. Prior to that, the introduction of line probe assays was a major step forward in drug susceptibility testing. The diagnosis of latent infection (LTBI) relied on the tuberculin skin test. Interferon-gamma release assays represent a major advance as they are more specific and can be performed in vitro and are logistically simpler. The current standard drug regimen takes 6 months of treatment, while treatment for drug resistant tuberculosis takes much longer and is associated with poor outcomes. This year, bedaquilin, the discovery of which was reported less than a decade ago [11], was recommended by the World Health Organization for the treatment of multidrug resistant tuberculosis. New candidate drugs in the pipeline such as PA824 and delamanid are well advanced in clinical trials. The BCG vaccine is widely used, provides good protection against serious childhood TB, but variable protection against pulmonary TB among adults. Given our lack of knowledge on correlates of protection, and limitations of animal models, vaccine candidates need to be tested in human trials. A trial in South Africa of one of these vaccine candidates (MVA85A) showed that in infants this vaccine provided no benefit if given after BCG, in comparison with infants who had received BCG only [12]. This disappointing result confirmed vaccine research is high risk. Yet, if successful, vaccines would have huge public health benefits and thus research needs to continue.
Where to go next?
Clearly, much more work is needed in the coming years to identify immunological correlates of progression to disease [13], to identify individuals who would benefit most from preventive therapy, or early TB treatment in candidates for cART. This knowledge would also be very helpful for vaccine development. Further development of point of care diagnostics is important to improve TB case finding in the general population and the early identification of (multi)drug resistance. New, shorter, drug regimens would be of enormous help to improve treatment outcomes in challenging circumstances [14]. And finally, an effective vaccine against pulmonary tuberculosis in adolescents and adults would be a game changer in tuberculosis control.
The evaluation of new tools will primarily be conducted in high burden, low- and middle- income countries. In these countries the need is greatest and evaluations can be performed in the most cost-effective way. However, there are constraints to such studies, such as limited clinical trials capacity, both in terms of human resources and laboratory capacity. Therefore, international collaboration is important to help overcome these constraints, provide technical and financial inputs, as well as links to centres of excellence in industrialized countries. In the Netherlands, even though financial resources for TB research are becoming more and more limited, an important contribution to international TB research is made through international collaboration in a range of areas, including immunology, genetics, microbiology, clinical medicine, pharmacology, and epidemiology. Given the nature of TB epidemiology in industrialized countries, including the Netherlands, with 70% of TB patients having been born abroad, additional funding for international TB research would not only be of global benefit, but also serve the interests of the population of high-income countries directly.
References
- Institute of Medicine. Ending Neglect. Washington DC: National Academy Press, 2000.
- Frieden TR, Fujiwara PI, Washko RM, Hamburg MA. Tuberculosis in New York City–turning the tide. N Engl J Med. 1995 Jul 27;333(4):229-33.
- Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997 May 3;349 (9061):1269-76.
- World Bank. Investing in Health. World Development Report 1993. New York: Oxford University Press, 1993.
- Corbett EL, Watt CJ, Walker N, Maher D, Williams BG, Raviglione MC, Dye C. The growing burden of tuberculosis: global trends and interactions with the HIV epidemic. Arch Intern Med. 2003 May 12;163(9):1009-21.
- Gandhi NR, Nunn P, Dheda K, Schaaf HS, Zignol M, van Soolingen D, Jensen P, Bayona J. Multidrug-resistant and extensively drug-resistant tuberculosis: a threat to global control of tuberculosis. Lancet. 2010 May 22;375(9728):1830-43.
- Dye C, Lönnroth K, Jaramillo E, Williams BG, Raviglione M. Trends in tuberculosis incidence and their determinants in 134 countries. Bull World Health Organ. 2009 Sep;87(9):683-91.
- Cole ST, Brosch R, Parkhill J, Garnier T, Churcher C, Harris D, et al. Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature. 1998 Jun 11;393(6685):537-44.
- Borgdorff MW, van Soolingen D. The re-emergence of tuberculosis: what have we learnt from molecular epidemiology? Clin Microbiol Infect. 2013 May 8. [Epub ahead of print]
- Boehme CC, Nabeta P, Hillemann D, Nicol MP, Shenai S, Krapp F, et al. Rapid molecular detection of tuberculosis and rifampin resistance. N Engl J Med. 2010 Sep 9;363(11):1005-15.
- Andries K, Verhasselt P, Guillemont J, Göhlmann HW, Neefs JM, Winkler H, et al. A diarylquinoline drug active on the ATP synthase of Mycobacterium tuberculosis. Science. 2005 Jan 14;307(5707):223-7.
- Tameris MD, Hatherill M, Landry BS, Scriba TJ, Snowden MA, Lockhart S, et al. Safety and efficacy of MVA85A, a new tuberculosis vaccine, in infants previously vaccinated with BCG: a randomised, placebo-controlled phase 2b trial. Lancet. 2013 Mar 23:381(9871):1021-8.
- Maertzdorf J, Weiner J 3rd, Kaufmann SH. Enabling biomarkers for tuberculosis control. Int J Tuberc Lung Dis. 2012 Sep;16(9):1140-8.
- Salomon JA, Lloyd-Smith JO, Getz WM, Resch S, Sánchez MS, Porco TC, Borgdorff MW. Prospects for advancing tuberculosis control efforts through novel therapies. PLoS Med. 2006 Aug;3(8):e273.


















































