Main content
Part 1 – Background & Burden
Introduction
Antimicrobial resistance (AMR) and antimicrobial stewardship (AMS) are no longer topics heard only occasionally. These topics are critical to global health and have gained justified, growing attention through policies, research and multiple structured and unstructured initiatives. While the numbers might be familiar – by 2050, 10 million people could die each year from AMR [1] – they may still feel abstract, even to healthcare professionals working in infectious diseases, microbiology or other AMR-related fields. What exactly is AMR, and what is its burden in sub-Saharan Africa? What is happening on the ground, and what has been implemented so far? What challenges do we face in addressing antimicrobial resistance or antimicrobial stewardship? Is the over-the-counter availability of antibiotics the main issue, or are there deeper root causes?
This article is the first in a series of two and explores these questions from a scientific perspective, complemented by personal observations.
Understanding antimicrobial resistance (AMR)
As we all know, practicing human medicine would not be possible without antibiotics, antivirals, antifungals, and antiparasitic medications. Antimicrobials are also essential in agriculture and animal health. When microorganisms no longer respond to antimicrobials that once killed them or suppressed their growth, we talk about antimicrobial resistance. It is not a new phenomenon; it is as old as the microbes themselves. It occurs when microorganisms interact with their environment and evolve survival mechanisms. Antimicrobial resistance is the most well-studied in bacteria and develops as the result of the acquisition, expression, and transfer of resistance genes. These genes can develop from spontaneous mutations or are acquired from other microorganisms or the environment. Simplified, under antimicrobial pressure, natural selection favors bacteria with resistance genes, which survive while susceptible bacteria die. Inappropriate antimicrobial use (in humans, animals and plants), inadequate access to clean water and sanitation, poor infection control, limited access to quality medicines and diagnostics, weak enforcement of regulations, and lack of knowledge and awareness all facilitate this selection process [2].
Attention to antimicrobial resistance has grown significantly during the past two decades. In
2015, the World Health Assembly adopted the first Global Action Plan on AMR, giving rise to a boost of national action plans on AMR worldwide, also in many sub-Saharan African countries. This was a much needed call, as global AMR mortality increased from 1990 to 2021 among people aged 5 years and older, with an increase of over 80% for the elderly. Resistance to last-resort antibiotics, carbapenems, also saw a substantial rise during this period [1]. Global antibiotic consumption increased by 65% between 2000 and 2015, with insufficient new antimicrobials in the pipeline [3,4]. Especially problematic are the Gram-negative bacteria, particularly Acinetobacter baumannii and Enterobacterales such as Escherichia coli, Klebsiella pneumoniae and Enterobacter species. However, rifampicin-resistant Mycobacterium tuberculosis and Gram-positives such as vancomycin-resistant Enterococcus faecium (VRE) and methicillin-resistant Staphylococcus aureus (MRSA) are also labeled as high-priority pathogens by the WHO [4]. Low- and middle-income countries are disproportionately affected by the antimicrobial resistance burden. In clinical settings in these countries, multidrug resistance in common hospital bacteria such as Klebsiella pneumoniae, Acinetobacter baumannii, and Pseudomonas aeruginosa results in serious treatment challenges.
According to the 2019 Global Burden of Disease Study, severe bacterial infections caused 13.6% of all global deaths, making them the second leading cause after ischemic heart disease. These deaths were associated with 33 bacterial pathogens, both resistant and susceptible to antibiotics, and primarily involved lower respiratory, bloodstream, and intra-abdominal infections. Antimicrobial resistance remains a challenge in these infections [5].
The burden of AMR in sub-Saharan Africa
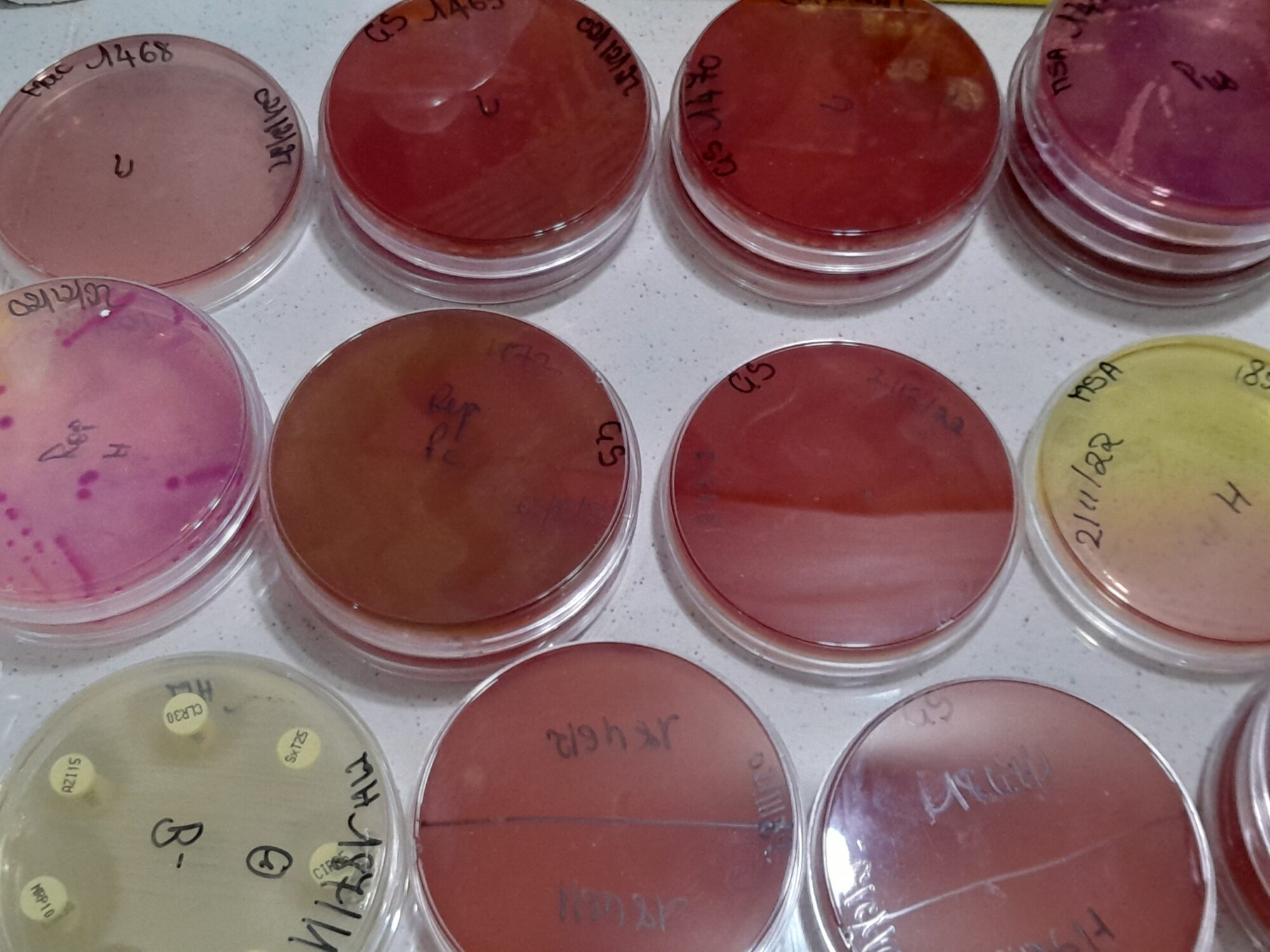
Through my work as a medical doctor and medical microbiologist at an urban tertiary hospital in Rwanda (since 2024), as well as in a smaller urban hospital in Ethiopia (2017-2023), and through visits to microbiology laboratories in other African countries, I have witnessed some of the burden of antimicrobial resistance in sub-Saharan Africa. Multidrug-resistant bacteria, especially extended-spectrum beta-lactamase (ESBL) producers, are detected on a daily basis in many of these laboratories. These bacteria are not only isolated from hospitalized patients, but also from patients coming from the community, pregnant women, neonates and patients admitted for elective surgery. The antimicrobial resistance rates that are encountered in Gram-negatives are alarming. Carbapenem resistance is not uncommon, particularly among inpatients, and some of these cases are very difficult to manage due to extensive resistance and limited access to last-line antibiotics. I have encountered both suspected and confirmed mortality related to antimicrobial resistance, as well as spread within departments leading to outbreaks, especially in intensive care units. Resistance genes are generally not known when treating patients in clinical settings. Unfortunately, the majority of the healthcare settings in the region lack (reliable) access to microbiology or molecular diagnostic laboratories [6]. In these settings, awareness of regional resistance patterns is critical to guide empirical reatment. However, community-level data and AMR-attributable mortality data is scarce in many African countries, as most studies are conducted in academic or tertiary care centers.
Patterns I observe in my current work in Rwanda are consistent with local data: more than one-third of Enterobacterales isolates are resistant to ceftriaxone and ciprofloxacin, while over half are resistant to trimethoprim-sulfamethoxazole, commonly used first-line antibiotics for many infections. Additionally, more than half of Acinetobacter isolates are carbapenem-resistant. Fortunately, MRSA and VRE remain relatively uncommon, which is reassuring given the limited availability of safe alternative therapies [7-11]. Community samples of humans, animals and their environment in rural Rwanda, suggest a widespread problem of resistance to first-line antibiotics among Gram-negative bacteria [9], and high resistance to first-line antibiotics was also found in Campylobacter isolates [12].
Findings from Ethiopia also reflect my personal observations in clinical practice. A systematic
review of data from 2009 to 2019 found that almost 50% of Staphylococcus aureus isolates were resistant to oxacillin (indicative of MRSA), and even 20% were resistant to vancomycin.
Resistance to amoxicillin/clavulanic acid exceeded 50% among important Gram-negatives, with ceftriaxone resistance reaching 74%. More than one-third of all Acinetobacter baumannii and Pseudomonas aeruginosa isolates were resistant to carbapenems [13]. These numbers might have worsened during the COVID-19 pandemic, a period when last-resort antibiotics were heavily overused.
While the exact AMR status in sub-Saharan Africa is largely undefined due to limited data and surveillance, the first global assessment of antimicrobial resistance in 2019 showed the region has the highest death rates worldwide from antibiotic-resistant infections, with the highest burden in West-Africa. In 2019, the burden of deaths from bacterial AMR in sub-Saharan Africa was higher than the number of deaths from HIV/AIDS and malaria [15]. The main driver is a high infectious diseases burden in the region linked to limited access to water and sanitation. There is persistent high mortality among children below 5 years, especially neonates, whereas AMR mortality has decreased for this age group across other regions in the world [16]. The high infectious diseases burden has led to abuse or misuse of antimicrobials in the human and veterinary sector, as there is limited regulatory enforcement and over-the-counter access to antimicrobials.
Beyond the limited availability of data, interpretation of available AMR data from sub-Saharan Africa requires caution due to quality problems and inconsistency. Antibiotics defined by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) or the Clinical and Laboratory Standards Institute (CLSI) are not consistently available, tested, or reported. Key methodological details needed for comparison and interpretation are often unclear or absent. Definitions for resistance patterns such as MRSA or ESBL are also frequently not provided. Additionally, discussions around antimicrobial resistance tend to focus primarily on antibiotic prescribing behavior, overlooking important environmental, agricultural, and other human factors. These include infection prevention and control, adequate diagnostics, quality of medications, antibiotics use and resistance in animals, and presence of resistance and antimicrobials in water, soil, or crops.
Comparison with AMR in the Netherlands
Although direct comparison is difficult, antimicrobial resistance rates from the Netherlands offer an interesting perspective, as human resistance data are well documented and accessible there. If bacteria produce ESBLs, they are resistant to antibiotics such as penicillin, cefazolin, ceftriaxone and cefotaxime. In 2023, ESBL-production was below 10% for E. coli and Klebsiella pneumoniae, with an exception for Klebsiella pneumoniae isolates found in ICUs (11%).
Carbapenem resistance is rare, with only 2% of Acinetobacter isolates being carbapenem-resistant [14]. The significantly lower rates are due to multiple factors, including strict policies and compliance to regulations across human, animal, food, and environmental sectors, as well as standardized treatment protocols and strong antimicrobial stewardship in clinical settings.
Encouraging developments
Sub-Saharan Africa has made – and continues to make – significant progress as awareness is
steadily improving, surveillance is strengthening, and antimicrobial stewardship activities are
being implemented. Global AMR mortality in children younger than 5 years has dramatically decreased during the last three decades, likely related to vaccination and access to WASH [1].
Opportunities and progress in the field, as well as on-the-ground challenges, will be explored
further in Part II.
M.J. Kreuger
MD Global Health, MSc Medical Microbiology
King Faisal Hospital Rwanda
Contributions by:
Marcel Ishimwe
Pharmacist
Founder AMR Initiative Rwanda
Musana Habimana Arsene
Biotechnologist
AMR Initiative Rwanda