Main content
Blount’s disease, bowlegs or tibia vara, is character-ized by proximal tibial bowing and endotorsion. It is a well-known condition in North America and Africa. The aetiology is still unclear. Mechanical loading and genetic predisposition are possible causes. The treatment often requires surgical intervention such as a proximal tibial osteotomy.
The deformity can be unilateral as well as bilateral with an even distribution of approximately 50%. [1] Consequences of the deformity of the limb, besides the obvious cosmetic aspects, are further deformation of the leg with possible gait deviations and limb shortening. This can lead to early onset arthritis of the knee. [2] The disease involves the epiphysis, physis and me-taphysis of the proximal tibia and results in a varus position, flexion and internal rotation of the lower limb (Figure 1). It was first described by Erlacher in 1917 and a more detailed descrip-tion followed by W.P. Blount in 1937.

Based on the age of onset different types of Blount’s disease can be distinguished. Onset of the disease before the age of 4 is named infantile Blount’s disease. Onset after this age, late-onset, can be divided into a juvenile (onset between age four to ten) and an adolescent type (onset after ten years of age). A pre-disposition has been reported in children of African descent. [2]
Blount’s disease is recognized on the conventional radiographs by the following typical features of the proximal tibia: tibia vara with the centre of rotation in the proximal epiphysis, metaphy-seal beaking, apparent fragmentation of the medial metaphysis adjacent to the epiphysis, straight lateral cortical wall of the proximal tibial metaphysis.[3] The radiographic progression of the disease can be classified according to Langeskiöld intosix stages (Figure 2), ranging from mild involvement with a beaked medial metaphysis (Stage 1) to the presence of a bony bar (Stage 6). The classification is used to aid diagnosis, to monitor the progression and to guide treatment.
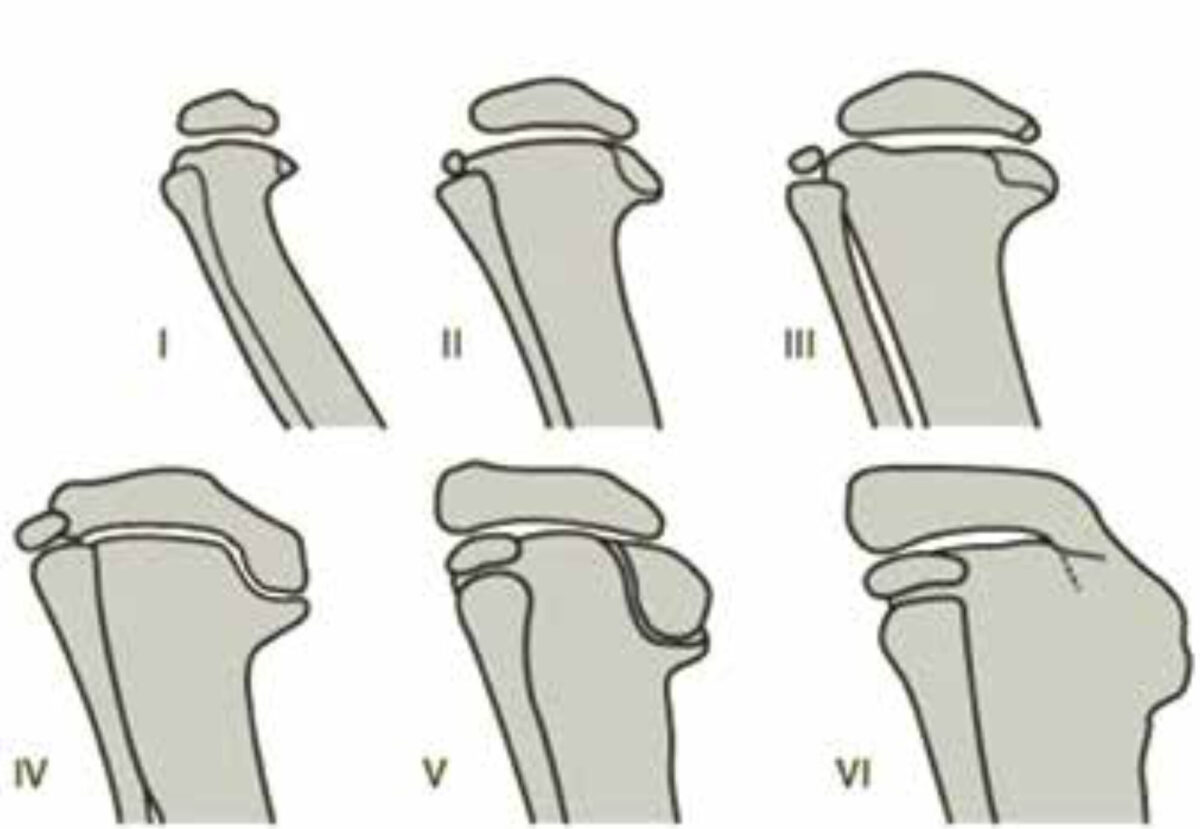
Stage I – Beaked metaphysis
Stage II – Saucer shaped defect
Stage III – Stepped defect
Stage IV – Bent physeal plate
Stage V – Double epiphysis
Stage VI – Medial physeal bar
Differential diagnosis bowlegs
The combination of the varus deformity and the internal tor-sion of the tibia is a consistent finding in Blount’s disease. This distinguishes Blount’s disease from its main differential diag-nosis in toddlers, the physiological genu varum, in which there is no increase of the internal torsion of the tibia. General condi-tions such as rickets can also cause varus deformity in the tibia but on the conventional radiographs Blount’s disease causes a sharp angulation at the site of the epiphysis, indicating a focal epiphyseal problem. A more gradual bowing is seen in general conditions such as rickets. To differentiate between the two, blood chemistry may help by showing low serum calcium, low serum phosphorus and high serum alkaline phosphatase in Rickets and normal blood counts in Blount’s disease.
Aetiology
The aetiology of Blount’s disease remains unknown up to now, but different hypotheses have been proposed and are discussed below.
Increased mechanical pressure on the knee joint
Development of the disease as a consequence of increased mechanical force is one of the most mentioned hypotheses of infantile Blount’s disease. It is based on the observed correlation between Blount’s disease and obesity. Further-more Blount’s disease is seen more often in children who walk at an earlier age. This theory, however, does not ex-plain the existence of a unilateral occurrence of tibia vara or the high incidence in African countries where there is a low prevalence of obesity. [2,4]
Nutrition
Some studies show that children with vitamin D defi-ciency are at a higher risk of developing Blount’s disease. [5] In a study conducted in Nigeria a variety of biochemical parameters in the serum of patients with Blount’s disease was compared with healthy subjects. They did not find significant differences in calcium, inorganic phosphate or copper concentration. Serum zinc levels and alkaline phosphatase, however, were significantly decreased in Blount’s. [6]
Genetics & heredity
Since in different cases a familial occurrence was found and Blount’s is more often seen in African and Afro-American children, a genetic component is also hypothe-sized. A genetic basis for Blount’s disease is mentioned in some case reports. The reports show siblings with Blount’s disease and no known risk factors, and healthy parents. The reports may lead in the direction of recessive inheritance.
Intra-articular changes and histology
Magnetic Resonance Imaging (MRI) of the knee in pa-tients with Blount’s disease show a thicker layer of epiphy-seal cartilage and increased height of the medial meniscus in the medial knee compartment. No difference was found with regards to the lateral meniscus. These macroscopic findings reflect the compensation mechanism of the me-dial down-sloping.
Histological analysis shows islands of densely packed hyper-trophied chondrocytes, areas of acellular cartilage matrix and abnormal clusters of capillaries resulting in necrosis of the physeal cartilage. There is disorganization of all structures on the medial side of the proximal tibial physis, but no bony bridges across the epiphysis are found. [7-11]
Treatment of Blount’s disease
Very mild deformities may resolve without treatment but for slight varus deformities (stages 1-2 Langenskiöld) conservative treatment with bracing or by repetitive plaster correction can be started. The pressure is transferred to the lateral compart-ment of the knee, stimulating the epiphyseal growth in the medial compartment.
Surgery is advised in the more severe stages (stages 3 or 4 Langenskiöld). Hemi-epiphysiodesis (permanent or revers-ible) is used to slow the growth on the lateral side and thereby correcting the deformity by the patient’s own growth. For reversible hemiepiphysiodesis the 8-plate (Orthofix) is used. The method is relatively easy, requires limited operative time, limited operative access and allows postoperatively full weight bearing. A figure-of-8 device is screwed above and below the epiphysis of the proximal tibia on the lateral side thus correct-ing the varus misalignment by allowing faster growth on the medial side. The internal rotational deformity is not corrected. In Blount’s disease a pretty high amount of implant failure is reported (26%).[12]
For the stages 5 and 6 different types of osteotomies are described. Opening- and closing-wedge osteotomies are both used, together with dome and Chevron-type osteotomies (V-type). Most of these osteotomies require internal fixation and the possibility of implant infection exists. Furthermore after consolidation implant removal is required. These techniques do not always successfully correct the rotational deformity that accompanies the angular, varus, deformity in this condition. The tibial W/M serrated osteotomy, first described in 1995 by Khermosh et al., enables simultaneous correction of the varus component as well as the torsional deformity, without the necessity for internal fixation. [13] The osteotomy is performed by making an M-shaped opening in the proximal tibia. Then the “teeth” of the M are disengaged and twisted correcting the varus and the rotational deformity. When the osteotomy is not stable a temporary Kirschner-wire can be introduced until the postoperative cast is set. A long-leg cast is worn for 8 weeks.
Besides the different osteotomies gradual corrections with external frames are described as well with the advantage of ad-justability, early weight-bearing and the ability to lengthen the limb. [14] The disadvantages of this technique are a longer con-solidation time and the need for expensive, complex devices. Complications include pin-track infections and postoperative neuropraxia. This technique appears to be more suitable for adolescents or adults in First World countries, because of the need for expensive devices and the pin-track problems.
Complications of treatment
After high tibial osteotomies the general complication rate is 13% and the recurrence rate is 57%. [15] Several complications have been described varying from non-union to nerve palsy. Specially the peroneal nerve is at risk in the lateral closing wedge osteotomies and in the corrections with an external frame. Non-union and delayed union occur often related to patient factors affecting his healing like sickle-cell anemia and malnutrition. Osteomyelitis can come about after wound heal-ing problems or surgical side infections. The odds of suffering an infection will depend on the circumstances in which the patient is operated. Certainly we have to take into account the hygienic circumstances of the hospital and the general health of the patient. Other complications are malunion, compart-ment syndrome, deep venous thrombosis, hematoma.
Recurrence of the deformity
After appropriate surgical correction of the varus malalign-ment in children with Blount’s disease sometimes the ma-lalignment reoccurs even after years. The recurrence rate seems to be related to the preoperative severity of the varus and to being overweight. Since we do not know what causes the disease and we do not treat the cause with the osteotomy the recurrence rate might be due to the on-going disease. There-fore monitoring of limb alignment and length is required until skeletal maturity. Future research should be focused on the underlying cause of Blount’s.
Conclusion
Blount’s disease is a well-defined deformity of the proximal tibia. It occurs mostly in children of African descent. It might be related to mechanical factors such as early walking age and obesity. Treatment is mainly surgical. Follow-up until skeletal maturity is mandatory.
References
- Birch JG, Blount disease. J Am Acad Orthop Surg 2013;21(7):408-18.
- Sabharwal S, Blount disease. J Bone Joint Surg Am 2009;91(7):1758-76.
- Langenskiold A, Tibia vara. A critical review. Clin Orthop Relat Res 1989;246:195-207.
- Langenskiöld A, Tibia vara: Osteochondrosis deformans tibiae: Blount’s disease. Clin Orthop Relat Res 1981;158:77-82.
- Montgomery CO, Young KL, Austen M, et al., Increased risk of Blount disease in obese children and adolescents with vitamin D deficiency. J Pediatr Orthop 2010;30(8):879-82.
- Giwa OG, Anetor JL, Alonge TO, et al., Biochemical observations in Blount’s disease (infantile tibia vara). J Nati Med Assoc 2004; 96(9):1203-7.
- Martinez AG, Weinstein SL, Maynard JA, Tibia vara: report of an unusual case. J Bone Joint Surg Am 1992;74(8):1250-6.
- Thompson GH, Carter JR, Late-onset tibia vara (Blount’s disease): current concepts. Clin Orthop Rel Res 1990;255:24-35.
- Thompson GH, Carter JR, Smith CW, Late-onset tibia vara: a comparative analysis. J Pediatr Orthop 1984;4(2):185-94.
- Carter JR, Leeson MC, Thompson GH et al., Late-onset tibia vara: a histopathologic analysis. A comparative evaluation with infantile tibia vara and slipped capital femoral epiphysis. J Pediatr Orthop 1988;8(2):187-95.
- Wenger DR, Mickelson M, Maynard JA, The evolution and histopathology of adolescent tibia vara. J Pediatr Orthop 1984;4(1):78-88.
- Schroerlucke S, Bertrand S, Clapp J et al., Failure of orthofix eight-plate for the treatment of Blount disease. J Pediatr Orthop 2009;29(1):57-60.
- Khermos O, Wientroub S, Serrated (W/M) osteotomy: a new technique for simultaneous correction of angular and torsional deformity of the lower limb in children. J Pediatr Orthop B 1995; 4(2):204-8.
- Price CT, Scott DS, Greenberg DA, Dynamic axial external fixation in the surgical treat-ment of tibia vara. J Pediatr Orthop 1995;15(2):236-43.
- Ferriter P, Shapiro F, Infantile tibia vara: factors affecting outcome following proximal tibial osteotomy. J Pediatr Orthop 1987;7(1):1-7.



















































