Main content
Many doctors from high-income countries (HIC) work in low- and middle-income countries (LMICs) for a limited period of time. The duration may vary from weeks in tar-geted and specialized missions, such as teams of ophthalmolo-gists or plastic surgeons, to months for others who are at registrar level to become, for example, a specialist in inter-nal medicine or paediatrics in HICs. For those in training for infectious diseases, this may lead to accreditation in tropical medicine; others e.g., in chest medicine focus on one disease such as tuberculosis. Finally, young doctors such as the Dutch Physician Global Health and Tropical Medicine (PGHTM) work for some years in rural or district hospitals in various capacities.
The training programme of the PGHTM is unique as it aims to train doctors in clinical medicine and public health with a particular focus on LMICs. It is a profes-sional career step, not an added-on training. It requires 2 ½ years of training after which doctors usu-ally serve for a minimum of 2-3 years in LMICs before returning home and continuing their career. The baseline clinical training in the Netherlands is well structured and focuses on surgery and obstet-rics & gynaecology (O&G) (9 months residency each, ‘clas-sical profile”); a minority train in O&G and paediatrics (9 months residency each, “mother-and-child profile”). A 3-month national tropi-cal course (NTC) is mandatory and includes clinical medicine, public health, health finance, health sys-tems, and ethical aspects, among other components.[1] Throughout the curriculum, 10 compulsory training days need to be attended, which focus on special topics such as transcultural rehabilita-tion, ophthalmology, and dental health. Lastly, a non-standardized 6-month residency in an LMIC setting follows with variable expo-sure and duties; the aim is to be better practically prepared before taking up a position in an LMIC.
What is the need for the pghtm – malawi as an example
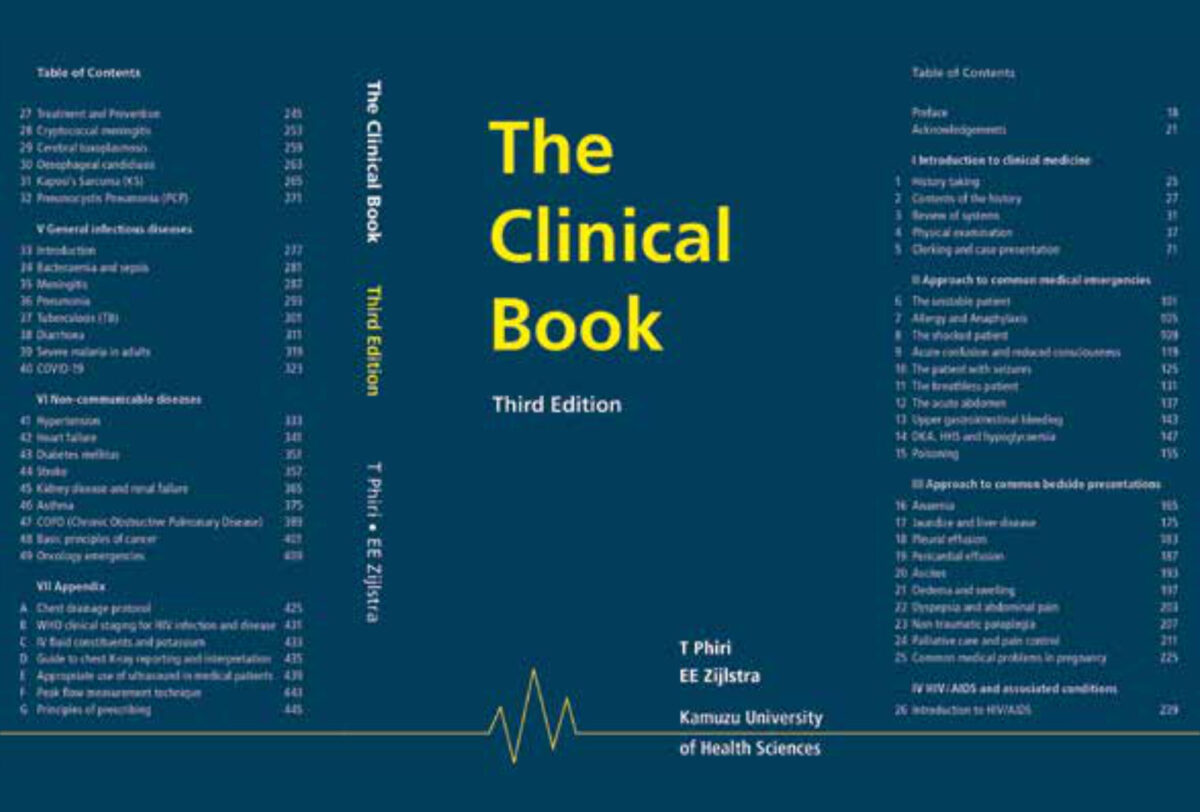
In Malawi, medical education leads to an MBBS degree (Medical Bachelor and Bachelor of Surgery), after a five-year curriculum at an accredited School of Medicine such as of the Kamuzu University of Health Sciences (KUHeS), formerly the College of Medicine, in Blantyre. After graduation, an internship (15 months) fol-lows with rotations in internal medicine, paediatrics, surgery, and obstetrics & gynaecology, each for 3 months. The last 3 months is mainly spent on public health. The intern is responsible for day-to-day care of patients in the wards and outpatient clinics and works under supervision of consultants and registrars (doctors in training to become consultants). After successful completion of the programme, the medical officer may be registered with the Medical Council and is allowed to practice independently.
What is required – tropical medicine: definition and changes since the year 2000
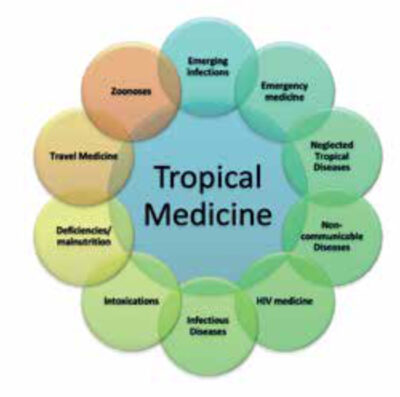
Tropical medicine traditionally referred to exotic, mainly vector-borne conditions, caused by parasites and occurring in warm climates. Examples are malaria, filarial diseases, sleeping sickness and helminthic infections.[2]
The HIV/AIDS epidemic, which started in the 1980s and that hit Africa disproportionally, completely changed priorities. Classical tropical diseases were overshadowed, and tropical medicine became, in the view of some, the medicine of immunosuppression.[3] A devastating tuberculosis (TB) epidemic followed in the wake of HIV/ AIDS. The HIV/AIDS epidemic not only required training doctors and nurses in antiretroviral treatment, but also brought about new and severe infections associated with HIV/AIDS such as bacterial meningitis, pneumocystis jerovicii pneumonia (PCP), and sepsis (pneumococcal, non-typhi salmonellae) as well as new or previously less common cancers such as Kaposi’s sarcoma and cervical carcinoma.
As world-wide most resources for research went to the big three (HIV/ AIDS, TB, and malaria), advocacy brought other groups of diseases to the forefront. The neglected tropical diseases (NTDs) are associated with poverty and lack proper diagnosis and treatment; there is a huge gap in research.[4] Other emerging infections include epidemics of dengue or chikungunya, while other outbreaks were more focal such as the Middle East respiratory syndrome (MERS), the severe acute respiratory syndrome (SARS – caused by SARS COV-1), and Ebola. Antibiotic resistance has become a major problem for the already lim-ited choice of antibiotics in LMICs.
The COVID-19 (caused by SARS COV-2) pandemic demonstrated the potential of rapidly spreading viral infections; other examples include influenza and avian flu with similar challenges in management and control. The COVID-19 pandemic showed how world-wide health systems may become over-whelmed by a new infection that hits LMICs hard and that uses up resources at the expense of other regular care.
Since 2010, the non-communicable diseases (NCDs) have been elevated onto national and global health and development agendas.[5] These include asthma, diabetes mellitus, hypertension, heart failure, and cancer, among others. NCDs cause 71% of all deaths, of which 77% are in LMICs.[6] While NCDs have been common in LMICs for decades, their importance was overshadowed by tropical diseases that needed proper diagnosis and treatment, while the (poor) management options for NCDs were taken for granted. Lately, western diet and lifestyle have become impor-tant additional risk factors. There is an overlap between infectious diseases and NCDs; for example, heart failure may be caused by HIV related infections (HIV, CMV) that cause myocarditis, or by rheumatic fever that causes valvular heart disease. Conversely, diabetes mel-litus is a risk factor for severe COVID-19 and melioidosis, among other; patients with cancer or malnutrition are at risk of various infections.
All the conditions mentioned above (classical tropical diseases, emerg-ing infections, NTDS, NCDs) are in the domain of internal medicine (and paediatrics) and require supervised clinical training for those who man-age these patients. (Figure 1) In LMICs, clinical expertise is provided in the central hospitals at the level of a specialist in internal medicine (UK: consultant physician; USA and Europe: internist). At the level of a district or mission hospital, adequate general training in curative medicine is required that includes internal medicine (as well as surgery, O&G and paediatrics – the “big four”); this applies to the locally trained doctor (as in Malawi) as well as the expat doctor. Figure 2 shows the level of knowl-edge required in internal medicine.
Ethical and professional aspects – implications for those preparing to work in the tropics
The medical profession is well regulated in the Netherlands and other high-income countries; in the Netherlands (NL), the doctor is registered with the Royal Dutch Medical Association and the registration needs to be renewed after 5 years. The registration allows medical practice only in the specialty or special profile (e.g., PGHTM) for which one is registered; this touches on professional aspects as well as eth-ics. This is also becoming the norm in LMICs. It follows that any expat doctor should have the same competencies in the 4 major specialties with adequate and sufficient clinical exposure and supervision (broad baseline training).
Alternatively, one could consider a single specialization such as O&G and working as a specialist (specialist train-ing). Another option would be training in e.g., the surgical specialties (surgery and O&G) or the medical specialties (internal medicine and paediatrics); this would require extended train-ing that does not reach the specialist level (dual limited specialist training).
The added value of the pghtm after returning to the netherlands
The question arises whether the PGHTM doctors are contributing to health care in NL after returning. This is difficult to assess both from a quantitative and qualitative point of view. While some continue to work in this field, others chose to continue their career in a new area and become general practitioners or clinical special-ists, or work in public health, e.g. in the municipal health service or other governmen-tal organizations, non-governmental organizations, the WHO, or research. Their contribution may depend on their clinical train-ing (homogenous, but restricted to surgery/O&G, or O&G/paediatrics – see above), the experience gained (heterogenous), and the scope of their current position.
It may be easier to define an optimal profile for the PGHTM aiming to work in LMICs and after returning to the Netherlands (Table 1). In conclu-sion, while surgical and obstetric skills remain important for the general medi-cal doctor in many settings, tropical medicine or medicine in the tropics has changed to include a dominant role for internal medicine, starting in the late 1980s with the HIV/AIDS epidemic (Figure 1). It follows that baseline train-ing should be broader and integrate adequate clinical training in internal medicine in the curriculum of the PGHTM, for an optimal contribution to health care in LMICs as well as health care in the Netherlands after returning.
CLINICAL
PUBLIC HEALTH
SPECIAL FOCUS ON
SPECIAL SKILLS
HICs: high income countries – LMICs: low- and middle-income countries – LGTB+: lesbian, gay, transgender, bisexual and other |
References
- www.oigt.nl
- Zijlstra EE. From Tropical Medicine to Global Health? MT bulletin 2017-2, vol 55.
- Moore EM. HIV is changing the face of tropical medicine. BMJ 2006, 332:1280.
- Pedrique B, Strub-Wourgaft N, Some C, et al. The drug and vaccine landscape for neglected diseases (2000-11): a systematic assessment. Lancet Glob Health. 2013 Dec, 1(6):e371-9. doi: 10.1016/S2214-109X(13)70078-0.
- NCDs NCD Alliance www.ncdalliance.org/what-we-do/what-are-ncds/ncds
- Noncommunicable diseases (who.int) www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases



















































