Main content
The rapid growth of childhood obesity rates is one of the most challenging public health problems in Mexico and other middle-income countries. Low-income groups living in rural communities of Mexico often consume processed, energy-dense foods of poor nutritional quality at relatively low prices.[1] Children from these communities are more likely to become overweight or obese and to develop micronutrient deficiencies as well. In addition, they are at risk of intestinal parasitic infection due to their poor sanitation and education.[2] Hence, children from these communities may have co-existing obesity, micronutrient deficiencies and intestinal parasitic infections.
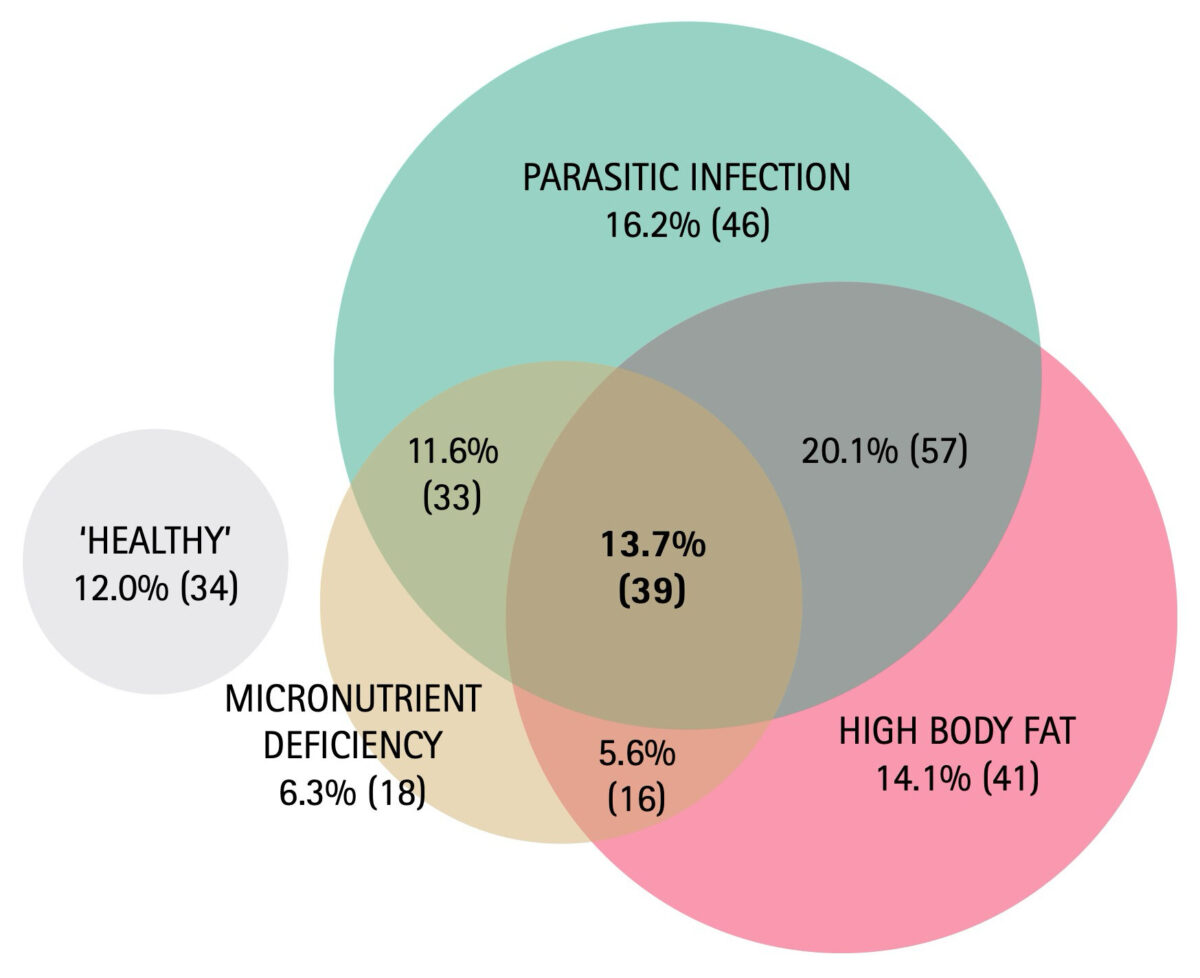
Obesity, micronutrient deficiencies and intestinal parasitic infections are ‘insults’ or stress factors that are associated with impaired development, systemic inflammation and metabolic changes in the short and long term.[3-5] The prevalence of each of these conditions was investigated in the global burden of disease study, which found that obesity (3.9%), micronutrient deficiencies (6.1%) and intestinal protozoa infection (5.7%) accounted for more than 10% of the global burden of disease.[3-5] Given the high rates in Mexico of overweight and obesity (more than 30% in children), micronutrient deficiencies (13% iron and 26% zinc deficiency) and parasitic infection (more than 50% of the population) [6-9], the large proportion of the Mexican population living in poverty (46% or 58 million) or in rural communities (20% or 25 million), and the possibility of a summative adverse effect on health of co-existing conditions, it is highly relevant to assess how many children have two or three of these conditions simultaneously. Thus, the objective of our study is to establish the proportion of children in rural Mexico living with co-existing micronutrient deficiency, high body fat and parasitic infection.
34% of the children had at least one micronutrient deficiency.
Materials and methods
Subjects and study design
A cross-sectional study was conducted involving a total of 301 primary school children (6-10 years of age), recruited from primary schools in two rural communities of El Marques in the State of Queretaro. The main ethnicity of the population is mestizo, and their main economic activity is agriculture. Caregivers received oral and written information about the study and provided informed consent. The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Human Research Committee of the School of Natural Sciences at the Universidad Autónoma de Querétaro (UAQ). Children’s parents or legal guardians (i.e. caregivers) were asked to attend their local health clinic to complete a medical history and a socioeconomic status questionnaire. Children who had received any deworming treatment in the previous four months or who had any physical or mental disability were excluded from the study.
Anthropometry and body composition
Weight and height were measured in duplicate in line with World Health Organization (WHO) guidelines. Weight was determined using a calibrated digital scale (SECA Mod. 813, Hamburg, Germany) and height was measured with a portable stadiometer (SECA Mod 206, Hamburg, Germany). Whole body composition was measured to determine body fat percent, using dual-energy X-ray absorptiometry (DXA) (Hologic Mod Explorer, Bedford, MA, USA). The cut-off point for high body fat (HBF) was 30% for girls and 25% for boys.
Intestinal parasitic infection
A direct copro-parasitological test consisting of a wet mount with iodine staining of slides was performed to screen and identify intestinal protozoa parasites, as described by WHO. A Kato-Katz smear (2 x 25 mg = 50 mg) was performed according to standard procedures to determine the presence of eggs of intestinal helminths. Children with helminth or protozoa infection were sent to the local clinic to receive treatment.
Micronutrient deficiency
Vitamin A, E and C blood levels were measured by reverse phase high pressure liquid chromatography (HPLC). Children with retinol concentrations <10 µg/dL were considered Vitamin A deficient, those with concentration of alpha-tocopherol <3 µg/mL were considered Vitamin E deficient, and children with concentrations of ascorbic acid <2 µg/mL were considered Vitamin C deficient. Furthermore, serum vitamin D was determined by a commercial 25 (OH)-Vitamin D direct ELISA kit (Immundiagnostik AG, Bensheim, Germany). Children with Vitamin D concentrations <50 nmol/L were considered Vitamin D deficient. Total iron concentration in serum was measured using a commercial kit (Iron Ferrozine, Elitech, Sées, France) and a spectrophotometer (Perkin Elmer, Mod Zeeman 5100). Children with iron concentrations <45 µg/dL were considered deficient. Zinc concentrations were measured in serum by atomic absorption spectrometry (AAnalyst 7000, Perkin Elmer Instruments, Norwalk, CT, USA). Zinc deficiency was defined as zinc plasma concentrations <65 mg/L. Children with any of the above micronutrient deficiencies (Vitamin A, E, C, D, total iron or zinc) were considered micronutrient deficient.
Results
Most of the children (88%) examined were from low or middle-low socioeconomic status households. We did not find differences in crowding, socioeconomic status or caregiver’s educational level among the children with none, one, two or three co-existing conditions. 34% of the children had at least one micronutrient deficiency; the most prevalent deficiencies were vitamin D (19%) and zinc (12%). 12% had more than one micronutrient deficiency. 53% of the children had at least one intestinal parasitic infection, the most prevalent being Entamoeba coli (22%), Endolimax nana (19%) and Ascaris lumbricoides (16%). 54% had high body fat. 12% had coexisting parasitic infection and micronutrient deficiencies, 20% had co-existing high body fat and parasitic infection, and 5.6% had co-existing micronutrient deficiency and high body fat. Most importantly, almost 14% of the children had all three conditions co-existing, i.e. micronutrient deficiency, parasitic infection, and high body fat (Figure 1).
Discussion
The percentages of children with two or three co-existing conditions are alarming. These children are at risk of systemic inflammation, impaired growth, poor intellectual development, chronic diseases and a summative negative effect on quality of life.[10,11] A clear example of this are micronutrient deficiencies, which not only cause specific diseases but also exacerbate infectious and chronic diseases, thereby increasing morbidity and mortality.[11]
The high prevalence of malnutrition and intestinal parasitic infection is likely to be related to poverty. The poorest people have a high risk of parasitic infection due to their lower level of education, poor sanitation and less access to health services.[2] Low-income groups living in rural communities in Mexico consume processed foods with heavy caloric content but poor nutritional quality. In our study region, they usually obtain their food from family-owned convenience stores that offer a wide range of calorie-dense foods and fried ‘junk’ food at relatively low prices. Children in particular are highly exposed to and influenced by visual cues present in these convenience stores – not only outside the store, where manufacturers of the main brands of ‘junk food’ advertise their products, but also on the shelf, where these ‘junk food’ brands advertise their products with promotions, plastic cartoon characters, and colourful labels (Figure 2). Other studies have associated the intake of these kinds of products (energy-dense and of low nutritional quality) with both obesity and micronutrient deficiencies.[12,13]
Given the high prevalence of co-existing malnutrition (i.e. high body fat and micronutrient deficiency) and parasitic infection, and the frequent co-existence of these conditions in the study population, there is a case to make for examining how widespread this problem is elsewhere in Mexico. Authorities and policy makers should be aware of these important public health problems. Strategies that have proven to prevent these problems in other settings and might be helpful for Mexico are decentralized public health policies including education, better living conditions including sanitation, programmes that promote healthy diets, and better access to healthy food.[2,14]
Conclusion
We found high prevalences of high body fat, micronutrient deficiencies, and intestinal parasitic infections as well as a frequent occurrence of these conditions simultaneously. Studies in other communities and municipalities in Mexico are needed to assess how widespread this problem is. Since the three conditions predispose to various diseases and disabilities, they need to be taken into consideration in future health and community programmes in Mexico.
Co-authors:
M. CAMPOS-PONCE & C. DOAK
DEPARTMENT OF HEALTH SCIENCES, FACULTY OF SCIENCE, VRIJE UNIVERSITEIT AMSTERDAM, THE NETHERLANDS
K. POLMAN
DEPARTMENT OF HEALTH SCIENCES, FACULTY OF SCIENCE, VRIJE UNIVERSITEIT AMSTERDAM, THE NETHERLANDS; DEPARTMENT OF BIOMEDICAL SCIENCES, INSTITUTE OF TROPICAL MEDICINE ANTWERP, BELGIUM
O.P. GARCÍA & J.L. ROSADO
DEPARTMENT OF HUMAN NUTRITION, FACULTY OF NATURAL SCIENCE, UNIVERSIDAD AUTÓNOMA DE QUERÉTARO, MEXICO
References
- L. Moreno-Altamirano, D. Hernandez-Montoya, M. Silberman, S. Capraro, J.J. Garcia-Garcia, G. Soto-Estrada, E. Sandoval-Bosh, [The nutrition transition and the double burden of malnutrition: changes in dietary patterns 1961-2009 in the Mexican socioeconomic context], Archivos latinoamericanos de nutricion 64(4) (2014) 231-40.
- S. Asaolu, I. Ofoezie, The role of health education and sanitation in the control of helminth infections, Acta tropica 86(2-3) (2003) 283-294.
- R. Black, Micronutrient deficiency: an underlying cause of morbidity and mortality, Bulletin of the World Health Organization 81(2) (2003) 79-79.
- M. Ng, T. Fleming, M. Robinson, B. Thomson, N. Graetz, C. Margono, E.C. Mullany, S. Biryukov, C. Abbafati, S.F. Abera, Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013, The Lancet 384(9945) (2014) 766-781.
- P.J. Hotez, M. Alvarado, M.-G. Basáñez, I. Bolliger, R. Bourne, M. Boussinesq, S.J. Brooker, A.S. Brown, G. Buckle, C.M. Budke, The global burden of disease study 2010: interpretation and implications for the neglected tropical diseases, PLoS Negl Trop Dis 8(7) (2014) e2865.
- M.C. Nesheim, M. Nestle, The Internationalization of the Obesity Epidemic, The Fight Against Hunger and Malnutrition: The Role of Food, Agriculture, and Targeted Policies (2015) 89.
- S. Villalpando, V.d.l. Cruz, T. Shamah-Levy, R. Rebollar, A. Contreras-Manzano, Estado nutricional de hierro, vitamina B12, folato, retinol y anemia en niños de 1 a 11 años: Resultados de la Ensanut 2012, Salud Pública de México 57(5) (2015) 372-384.
- E. Diaz, J. MONDRAGON, E. Ramirez, R. Bernal, Epidemiology and control of intestinal parasites with nitazoxanide in children in Mexico, The American journal of tropical medicine and hygiene 68(4) (2003) 384-385.
- L. Quihui, M.E. Valencia, D.W. Crompton, S. Phillips, P. Hagan, G. Morales, S.P. Díaz-Camacho, Role of the employment status and education of mothers in the prevalence of intestinal parasitic infections in Mexican rural schoolchildren, BMC Public Health 6(1) (2006) 1.
- G. Zavala, K.Z. Long, O.P. Garcia, C. Caamano Mdel, T. Aguilar, L.M. Salgado, J.L. Rosado, Specific micronutrient concentrations are associated with inflammatory cytokines in a rural population of Mexican women with a high prevalence of obesity, The British journal of nutrition 109(4) (2013) 686-94.
- T.H. Tulchinsky, Micronutrient deficiency conditions: global health issues, Public Health Reviews 32(1) (2010) 243.
- R. Rosenheck, Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk, Obesity Reviews 9(6) (2008) 535-547.
- S.A. Bowman, B.T. Vinyard, Fast food consumption of US adults: impact on energy and nutrient intakes and overweight status, Journal of the american college of nutrition 23(2) (2004) 163-168.
- M. Flynn, D. McNeil, B. Maloff, D. Mutasingwa, M. Wu, C. Ford, S. Tough, Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with ‘best practice’recommendations, Obesity reviews 7(SI) (2006) 7-66.

















































