Main content
Ultrasound imaging is commonly used for prenatal screening. In recent years, the cost of ultrasound devices has decreased to a few thousand dollars and devices have become more portable, with possibilities for connection to laptops, tablets or smartphones.
Whereas in high-income countries ultrasound imaging in obstetrics focuses nowadays on foetal abnormalities (such as foetal growth restriction and structural abnormalities), it is often used for different purposes in low-income countries. These countries use ultrasound for pregnancy dating and diagnosing twin pregnancies and placenta praevia, to identify high-risk pregnancies, and to ensure optimal birth care. The WHO recommends an ultrasound scan for pregnant women in resource limited settings for accurate gestational age estimation, for detection of multiple pregnancies, foetal malpresentation, foetal anomalies, placenta praevia and polyhydramnios, for confirming foetal viability, and for improvement of a women’s pregnancy experience.[1]
Unfortunately, ultrasound imaging still remains out of reach for most pregnant women in these settings. This is caused mainly by a severe shortage of trained sonographers, who are needed to both acquire and interpret the ultrasound images.[2,3] Depending on the formal diploma or course, training a sonographer can take months to years and forms a barrier to implementation of prenatal ultrasound imaging in these countries. In this article, we present a system that can automatically interpret ultrasound images using deep learning. By combining this with a standardized acquisition protocol that can be taught to midwives within two hours, it could be possible to widely implement prenatal ultrasound imaging in resource-limited settings.
The standardized ultrasound acquisition protocol
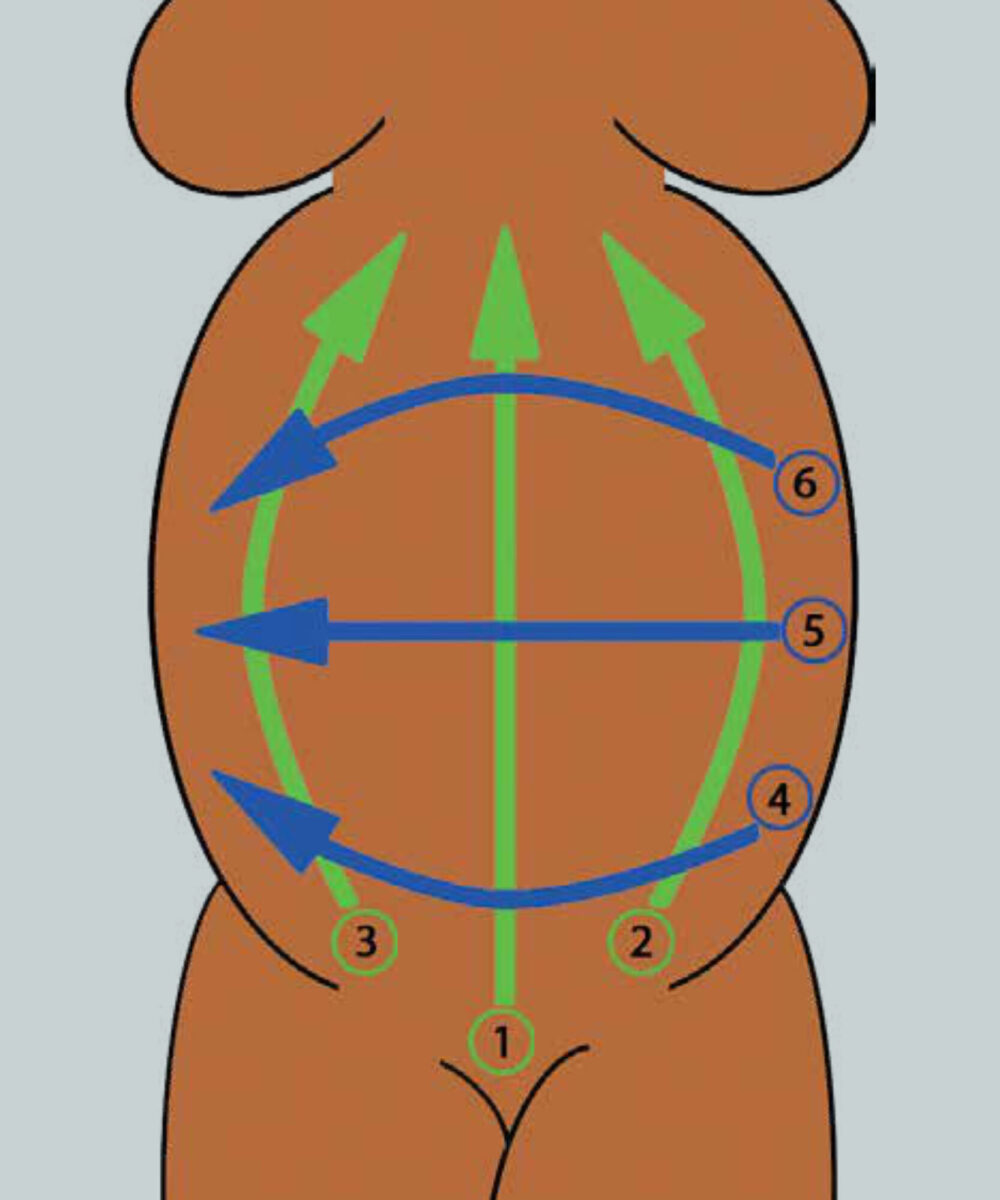
DeStigter et al. developed the obstetric sweep protocol (OSP), which is particularly suitable in rural areas.[4] The OSP consists of six predefined sweeps with the ultrasound transducer over the abdomen of the pregnant women (Figure 1). In their paper they mention: ‘These sweeps can be learned by an untrained person with limited knowledge of internal anatomy in a few hours’. To put their claim to the test, we organised a workshop for five midwives at St. Luke’s Catholic Hospital in Wolisso, Ethiopia in 2019. We were able to demonstrate that the OSP can indeed be taught to midwives without any prior knowledge of ultrasound within two hours.
Automated ultrasound interpretation using deep learning
Deep learning is a machine learning technique that can be used to develop computer algorithms that can automatically perform tasks. This technique has become popular in recent years and is already used for various applications like speech recognition, natural language processing, and facial recognition. Since 2013, deep learning has also been successfully applied in the field of medical imaging.[5] We combined deep learning algorithms with the OSP in order to eliminate the need for a trained sonographer to interpret the ultrasound images. A large dataset was required for the development of these algorithms. The OSP was therefore performed on more than 300 pregnant women at St. Luke’s Catholic Hospital. This data was then used to develop the deep learning algorithms. The developed algorithms were used for three different applications: determining foetal presentation, detecting twin pregnancies, and determining gestational age by estimating the foetal head circumference.[6]
Clinical implications
The OSP makes it possible to train midwives to use ultrasound in resource-limited settings within two hours. The combination of the OSP and the automated ultrasound interpretation would make prenatal ultrasound imaging much cheaper and easier to implement and has therefore the potential for widespread use in resource limited settings. Additionally, it is very important to carefully consider how patient management and follow-up are taken care of when these risks are detected in resource-limited settings. The automatically estimated gestational age could be used to manage pregnancy complications appropriately and refer high-risk pregnant women to a health care facility in a timely fashion. There are studies showing that ultrasound imaging increases antenatal care clinic visits [7,8] and even has the potential to decrease maternal mortality,[9] but there are also studies showing that ultrasound screening alone does not address barriers to referrals.[10] A recent cluster randomised trial found no effect of routine antenatal ultrasound, although in this study 43% of women in the control group who were not supposed to receive an ultrasound still received it.[11]
Conclusion
In implementing ultrasound imaging, it is clear that training of health care workers to appropriately use ultrasound imaging is essential for success. We are planning further studies to investigate whether automated interpretation, which makes the use of ultrasound imaging much easier, will be able to realise its potential benefit in resource-limited settings.

References
- World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience Luxembourg; 2016. https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf
- Kim ET, Singh K, Moran A, Armbruster D, Kozuki N. Obstetric ultrasound use in low and middle income countries: a narrative review. Reproductive Health 2018;15(1):129.
- LaGrone LN, Sadasivam V, Kushner AL, Groen RS. A review of training opportunities for ultrasonography in low and middle income countries. Trop Med Int Health 2012;17(7):808-19.
- DeStigter KK, Morey GE, Garra BS, et al. Low-cost teleradiology for rural ultrasound. In IEEE Glob Humanit Technol Conf;2011:290-95.
- Litjens G, Kooi T, Ciompi F, et al. A survey on deep learning in medical image analysis. Medical image analysis 2017;42:60-88.
- Van den Heuvel TLA. Automated low-cost ultrasound: improving antenatal care in resource-limited settings. Doctoral dissertation; 2019. Radboud University, Nijmegen, Netherlands.
- Ross AB, DeStigter K, Rielly M, et al. A low-cost ultrasound program leads to increased antenatal clinic visits and attended deliveries at a health care clinic in rural Uganda. PLOS ONE 2013;8(10):e78450.
- Cherniak W, Anguyo G, Meaney C, et al. Effectiveness of advertising availability of prenatal ultrasound on uptake of antenatal care in rural Uganda: A cluster randomized trial. PLOS ONE 2017;12(4):20175440.
- Stanton K, Mwanri L. Global Maternal and Child Health Outcomes: the role of obstetric ultrasound in low resource settings. J Prev Med 2013;1(3):22-29.
- Franklin HL, Mirza W, Swanson DL, et al. Factors influencing referrals for ultrasound-diagnosed complications during prenatal care in five low and middle income countries. Reproductive Health 2018;15(1):204.
- Goldenberg RL, Nathan RO, Swanson D, et al. Routine antenatal ultrasound in low-and middle-income countries: first look a cluster randomised trial. BJOG 2018;125(12):1591-99.


















































