Main content
The World Health Organization has stated that ‘Climate change is the greatest challenge of the 21st century, threatening all aspects of the society in which we live. The impacts of climate change include thawing of permafrost, coastal erosion, increases in droughts, floods and heatwaves, risks to infrastructure and food security, and the arrival of new diseases. [1] Climate change affects human health in two ways: there is a direct effect (heat waves, air pollution, storms and floods) and an indirect effect through expansion of mosquito populations (vector-borne diseases such as malaria, dengue), contamination of water (food-borne disease), and deterioration of environmental conditions. [2]
Models indicate that climate change is not the only factor but that other anthropogenic (man-made) factors also contribute, including socio-economic transformation, human population growth, habitat reduction including deforestation, land use modification and fragmentation (‘wild’ vs human land use), and change in biodiversity. [3]
The combined effect of these factors may be summarized as follows:[4]
- Increased risk of introduction and endemic transmission of exotic diseases from around the world, either direct or vector-borne, such as Severe Acute Respiratory Syndrome (SARS)
- Re-emergence of endemic diseases, such as West Nile Virus disease, Lyme disease and other vector-borne infections in the Americas
- South-to-North spread of disease by increasing vector ranges
The impact of this may be aggravated by the aging populations in which chronic diseases are common.
Climate change and vector-borne diseases
In the past decade, new diseases have (re)-emerged such as Middle East Respiratory syndrome caused by coronavirus (MERS-CoV) in the Middle East, and ebola in Africa. Other vector-borne diseases spread from their endemic areas; for example, spread to the Americas occurred in the case of dengue (from Asia and the Caribbean) and chikungunya, Zika and yellow fever (from Africa). While the incidence of food-borne, water-borne and air-borne diseases may be increase due to climate change, the principal focus globally is on the increase of mosquito-borne diseases that are responsible for 212 million cases per year (malaria, dengue, chikungunya, Zika virus disease). [3]
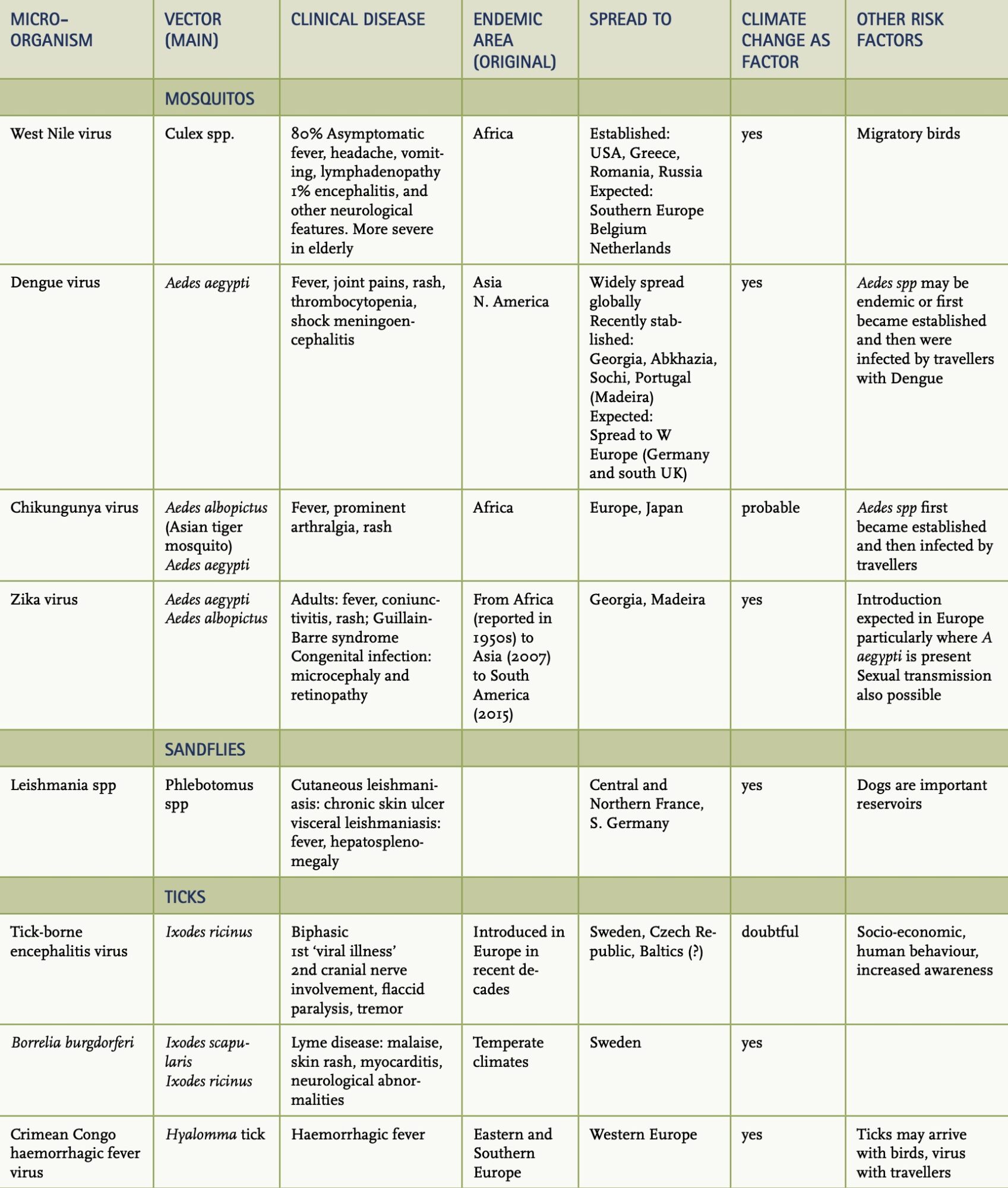
The main epidemiological and clinical aspects of mosquito and other vector-borne disease are summarized in Table 1.
Aedes aegypti is the most important vector in this context; it transmits viruses that cause dengue fever, chikungunya, Zika, and yellow fever.
Dengue is globally the most important arboviral infection. In recent years, the disease has spread beyond the main endemic areas (Asia, Caribbean) to virtually all continents with half of the global population at risk. Classically the vector is Aedes aegypti, but in recent years Aedes albopictus has become a competent vector and has become established in Europe. This is thought to be caused by an increase in their geographic ranges, but genetic changes of these viruses also occur that make them adaptable to animals and possibly facilitate human-to-human transmission. [4] Mapping suggest that further expansion of Aedes aegypti will occur in Southern Europe with possible spread to Western Europe including Germany and the South of the UK, based on increased temperatures and rainfall. Besides increased temperatures, flooding, urban migration and subsequent overcrowding are also risk factors for dengue outbreaks.
There is no effective vaccine. Intensive vector control is applied with new options for innovative approaches. The intracellular bacteria Wolbachia, which interferes with viral replication, has been successfully introduced in wild Aedes mosquito populations. The first results look promising, and the result of formal studies in Indonesia and Vietnam that measure the efficacy are eagerly awaited. [5]
Dengue was followed by chikungunya, a disease that was practically unheard of except in East Africa and has spread widely to the Old and New World. It has now been transmitted, for example, to Japan and Europe, supposedly because of the spread of the vector as the result of climate change.
Zika also originated from Africa and spread to Micronesia and French Polynesia between 2007 and 2014, causing thousands of cases. In 2015, it was introduced in Brazil and spread further to most regions in South and Middle America, with 1.5 million cases in Brazil alone. Up to 8000 cases of congenital neurological malformations have been reported such as microcephaly, as well as retinal abnormalities such as macular and optic nerve atrophy. [6]
Higher temperatures are not always responsible for vector spread and increased frequency of disease. Tick-borne encephalitis is caused by the Ixodes ricinus tick that in Sweden feeds on roe deer. After the massive death of deer during a harsh winter, the ticks fed on small rodents that are likely to be more viraemic and thus infectious to ticks with an increase in numbers of human cases. [7]
The effect of climate change itself and its effect on vectors is even more complex. Infections that are known to appear as major outbreaks after heavy rainfall include Ross River fever and Murray tick encephalitis in Australia and Japanese encephalitis in South-East Asia. [2] The risk of spread of the vector range is not linear. For Ross River Fever, the optimum temperature 26.4 °C; when temperatures reach the thermal limits, i.e. decrease below 17 0C or increase above 37.5 °C, transmission no longer occurs. This explains why in temperate climates the disease is seasonal. With increasing global temperatures, the disease may spread to non-endemic areas, whereas in other areas transmission may stop if temperatures were already near the thermal limit. [8]
It is interesting to consider the effect of climate change on helminthic infections. For schistosomiasis, the hotter and dryer climate changes may reduce the snail vector population, which, together with mass drug administration and the possibility of a vaccine, may reduce the incidence of this disease. On the other hand, for lymphatic filariasis, climate change may expand vector ranges and breeding seasons, with increased incidence as a consequence. [9] With regard to soil-transmitted helminths, Ascaris lumbricoides will remain important, while ancylostomiasis (particularly hookworm) is expected to become the dominant species in Africa. [9]
Climate change may also promote proliferation of an existing vector such as Anopheles spp. in previously malaria endemic areas such as the UK or the Netherlands, with the theoretical risk of re-introduction of malaria. The outbreaks of P. vivax in Greece (2009-2012) were however thought to be the result of introduction by travellers. [10]
Non-communicable diseases (ncds) and climate change: is there any relation?
NCDs are responsible for 70% of global deaths and this number is expected to rise. [11] There are parallels between climate change and NCDs; both are preventable, largely caused by human behaviour and they require a multisectoral response. Both are global disasters for which solutions are available; these require leadership and diversion of funds. [11]
Many impacts of climate change on body systems are still poorly understood. One potential impact is in kidney disease, where dehydration may cause blood hyperosmolarity and reduced kidney perfusion. Heat stroke may cause rhabdomyolysis (breakdown of muscle) with direct effect on kidney function. Poor hydration may predispose to kidney stones and urinary tract infection. [12]
An impact on mental health has also been suggested directly via heat stress or indirectly, for example via economic loss, threats to health and well-being.[13]
The effect of climate change has so far focussed on increasing temperatures and the effect of heat on mortality. One review that was mainly restricted to urban areas and did not include Africa or the Middle East showed that mortality caused by cold is greater than that caused by heat, as defined as temperatures below and above optimum temperature. This is thought to be due to (non-communicable) cardiovascular or respiratory disease. Temperature-attributable deaths caused by cold and heat were 7.2% and 0.42%, respectively. The effect of extreme heat (heatstroke) or cold (hypothermia) contributed < 1%. These observations suggest that various climate change scenarios should be taken into account in policy making and adaptation measures. [14]
Conclusion
While the effects of climate change on health are unmistakable, increasing insight shows that other factors socio-economic and ecological factors as well as urbanization – may be equally important. Vector-borne infectious diseases are likely to become more common in endemic areas as well as in non-endemic areas due to the increasing range of vectors. Other infectious conditions may become less common. The effects on non-communicable diseases are not yet fully understood.
While the incidence of food-borne, water-borne and air-borne diseases may increase due to climate change, the principal focus globally is on the increase of mosquito-borne diseases that are responsible for 212 million cases per year.

















































