Main content
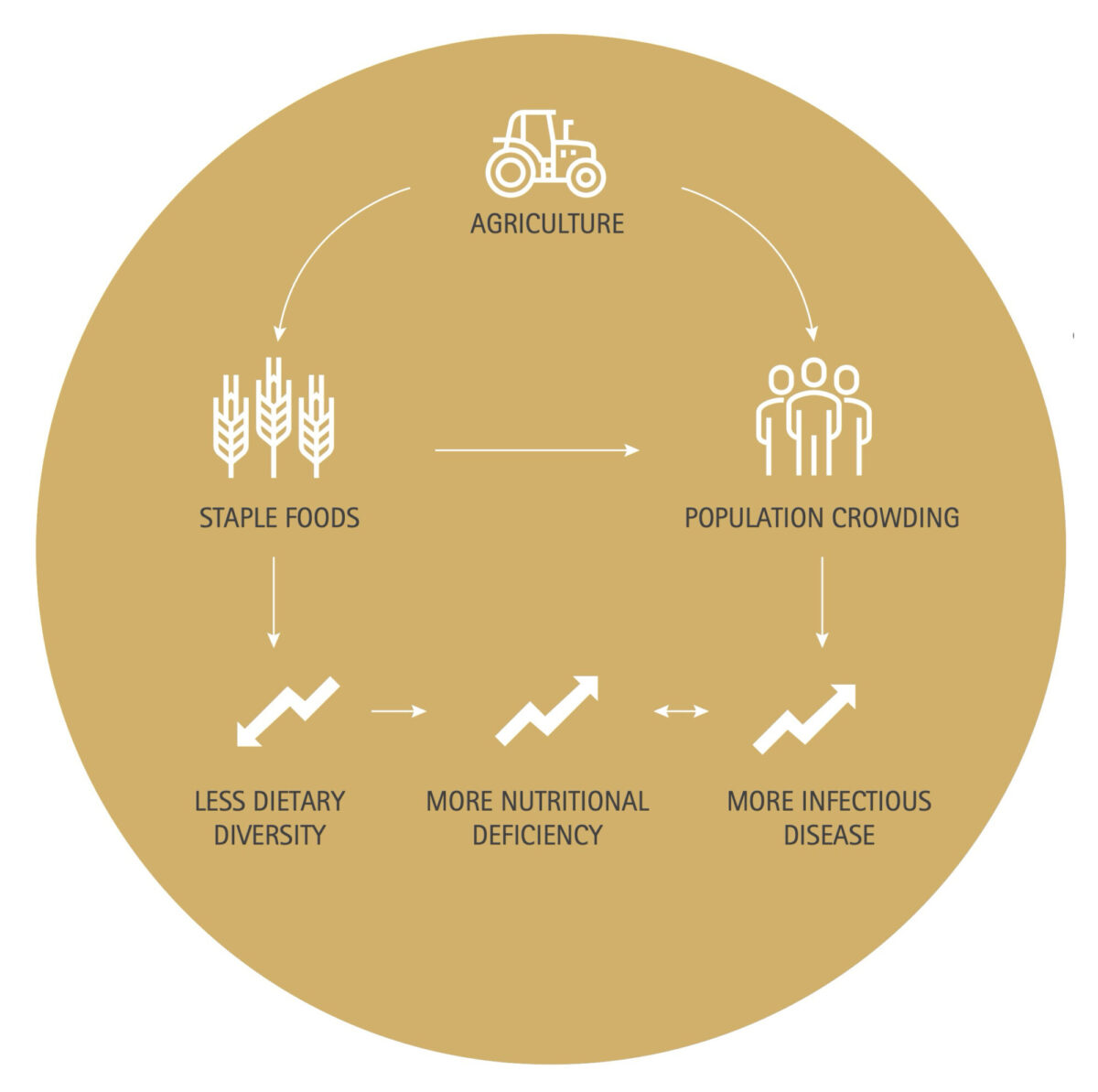
The shift from hunter gatherer to agricultural societies brought two fundamental changes in human diet and social structures. First, by producing surplus grains, agriculture stimulated population growth and greater population density, contributing to infectious disease. Secondly, because early agricultural societies were largely reliant on a limited number of staple grains, the diet became less diverse and of poor nutritional quality as compared to previous hunter gatherer societies. Figure 1 is a simplified schematic explaining why, historically, the shift from hunter gatherer to agricultural societies contributed to an increase in nutritional deficiency and infectious disease. These patterns are verified in the archaeological record, in which the emergence of agricultural societies coincides with evidence for nutritional deficiencies and infectious disease.
In addition to their historical convergence, poor nutrition and infectious disease are also intertwined due to additional complex biological interactions. This article focuses on the history of one of the seminal topics in the field of nutrition and infectious disease, specifically the relationship between infections and anaemia. In this overview, I begin with the archaeological evidence linking anaemia with infectious disease and then shift to the modern public health context of iron-deficiency anaemia caused by infectious disease. Finally, I discuss anaemia in relation to obesity, triggered by the inflammation stimulated by adipocytes, contributing to a pattern of obesity & micronutrient deficiency co-existing in many countries where infectious disease is highly prevalent.
Anaemia in ancient Peru
Until the last decade, archaeologists identified anaemia through malformations of the skull, known as porotic hyperostosis and cribra orbitalia. Porotic hyperostosis is an expansion of the bone marrow (hyperostosis) combined with bone pitting (porotic bones) on the sides of the parietal and temporal bone of the skull. Cribra orbitalia is a similar porous expansion, as seen with porotic hyperostosis, but located at the orbits (eye socket). These changes in skeletal remains were identified more than five decades ago as being consistent with the cranial bossing that is seen in genetic anaemias such as beta thalassemia.[2] More recent studies have also shown patterns in the occurrence of cribra orbitalia, corresponding to anaemia related to malaria.[3,4] Given the similarities in the physiological response and the co-occurrence in the archaeological record, porotic hyperostosis and cribra orbitalia were both seen as indicative of anaemia. In South America, bio-archaeologists have wondered why these skeletal malformations occurred so frequently in pre-Columbian populations. What was the cause? In answering this question, archaeologists focused first on dietary causes, especially iron deficiency. Specifically, the cause was assumed to be related to the dependency on plant-based diets. Along with the onset of agriculture, early populations became reliant on a diet rich in the plant fibres (e.g. phytates) that inhibit the absorption of non-haeme sources of iron (i.e. iron from plants).
In the early 1990s, Stuart-Macadam [5] added to the debate by calling attention to the known relationship between inflammation and anaemia, drawing the attention of bio-archaeology to the anaemia of inflammation. She argued that the porotic hyperostosis and cribra orbitalia found in past populations were likely to have been caused by infection through biological mechanisms stimulated by inflammation. This process, known as the iron withholding mechanism, is part of the immune response, stimulated by interleukin 6 (IL-6). This mechanism maintains iron stores while withholding iron from parasites such as Plasmodium, which thrive in an iron-rich environment. Stuart-Macadam argued that the iron withholding response could explain the anaemia, but also included it as a vital evolutionary response protecting early humans against parasitic infections such as malaria. As a Master’s student, I explored whether porotic hyperostisis and cribra orbitalia could be explained by infection. I considered whether a specific malaria-like endemic disease caused by B. bacciliformis could be an explanation for the anaemia found in pre-Columbian Peru. Ultimately, the explanation did not fit the biology of the disease itself. The phase of the disease which would have triggered an inflammatory response has a >90% mortality rate. Few survivors would have displayed the bone changes that are found in the archaeological record, as these are most likely to occur during the recovery phase.
However, in delving into the early history of anaemia and the thinking about anaemia amongst bio-archaeologists, I became aware of and interested in the complex biological relationships between nutrition and infectious disease. Since my days as a Master’s student in anthropology, the thinking in archaeology has changed. Now, porotic hyperostosis and cribra orbitalia are thought to be distinct conditions, reflecting nutritional deficiency and infectious disease respectively. Walker et al [6] proposed the theory that porotic hyperostosis is largely caused by a deficiency of one or more of the water soluble vitamins, such as folate, B-12 or vitamin C, but is not related to iron deficiency. They argue that the bone changes of porotic hyperostosis are more in line with megaloblastic forms of anaemia, such as pernicious anaemia from B-12 or folate deficiencies. Cribra orbitalia, on the other hand, occurs in patterns more closely related to infectious disease. In spite of the change in the thinking about the aetiology, archaeologists agree that both conditions co-existed largely because infection and undernutrition also coincided historically.
Lower-income populations in low and middle income countries are also increasingly at risk of obesity.
Iron deficiency and malaria: complex public health issues
The connection between anaemia and infectious disease continues to be an important concern. While some parasites directly contribute to anaemia by parasitizing and rupturing the blood cells, parasites that trigger the IL-6 response contribute to iron deficiency anaemia through the anaemia of inflammation described above. Furthermore, some parasitic infections that cause intestinal bleeding, such as hookworm, contribute to iron deficiency anaemia through blood loss. In addition, infections that cause diarrheal symptoms limit the absorption of nutrients while also increasing nutritional losses. Together, these relationships explain multiple pathways through which infections contribute to both anaemia and iron deficiency. In malaria endemic areas, these relationships lead to complex public health questions related to where and when iron supplements are appropriate. Although iron is important to immune functions [7], studies have shown that high iron (serum ferritin) at baseline was associated with an increased risk of malaria (Plasmodium falciparum) at follow-up.[8] Supplements can increase the risk associated with some parasites by providing an iron-rich environment. In a review of the evidence, the WHO Consultation on prevention and control of iron deficiency in infants and young children in malaria endemic areas advised against wide-scale iron supplementation in malaria endemic areas.[9]
Obesity contributing to anaemia
The anaemia of chronic inflammation is also referred to as the anaemia of chronic disease due to the prolonged inflammatory responses related to overweight or obesity. In the past, the anaemia of chronic disease was a concern of wealthy countries or of higher-income populations within low and middle income countries. However, due to changes in the economy and the food supply, known as the nutrition transition [10], lower-income populations in low and middle income countries are also increasingly at risk of obesity.[11] Thus, the populations that are most at risk for the anaemia of chronic disease are most likely to be consuming foods that are energy dense but of poor nutritional quality, also resulting in a diet poor in iron. Due to these patterns, iron deficiency anaemia is exacerbated by a combination of inflammatory responses related to increases in body fat, changes in the global food supply and, in countries where parasites remain endemic, infectious disease.

References
- Cohen MN and Armelagos GJ. Editors. 1984 Paleopathology at the Origins of Agriculture. Orlando, FL: Academic Press.
- Angel JL. Porotic hyperostosis, anemias, malarias, and marshes in the prehistoric Eastern Mediterranean. Science. 1966 Aug 12;153(3737):760-3.
- Rabino Massa E, Cerutti N, Marin A, Savoia D. Malaria in ancient Egypt: paleoimmunological investigation on predynastic mummified remains. Chungara 2000. 32:7-9.
- Smith Guzmán NE, The skeletal manifestation of malaria: An epidemiological approach using documented skeletal collections, Am J Phys Anthropol. 2015 158, 4, (624-635), (2015).
- Stuart-Macadam P. Porotic hyperostosis: a new perspective. Am J Phys Anthropol. 1992 Jan;87(1):39-47.
- Walker PL, Rhonda R, Bathurst RR, Richman R, Gjerdrum T & Andrushko VA The causes of porotic hyperostosis and cribra orbitalia: a reappraisal of the iron-deficiency-anaemia hypothesis. Am J Phys Anthropol. 2009 Jun;139(2):109-25. doi: 10.1002/ajpa.21031.
- Beard JL. Iron Biology in Immune Function, Muscle Metabolism and Neuronal Functioning. J Nutr. 2001. 131, 2 (1): 568S-580S.
- Moya-Alvarez V, Cottrell G, Ouédraogo S, Accrombessi M, Massougbodgi A, Cot M. Does Iron Increase the Risk of Malaria in Pregnancy? Open Forum Infect Dis. 2015 Mar 20;2(2)
- World Health Organization. Conclusions and recommendations of the WHO Consultation on prevention and control of iron deficiency in infants and young children in malaria-endemic areas. The United Nations University. Food Nutr Bull. 2007 Dec;28(4 Suppl):S621-7.
- Popkin BM. Nutritional patterns and transitions. Popul Dev Rev. 1993;19(1):138-157.
- Monteiro CA, Moura EC, Conde WL, Popkin BM Socioeconomic status and obesity in adult populations of developing countries: a review. Bull World Health Organ. 2004 Dec; 82(12):940-946.

















































