Main content
There is a global need for affordable prostheses. An estimated 0.5% of the global population in low- and middle-income countries (LMICs) requires prostheses or orthotics according to the World Health Organization and the International Society for Prosthetics and Orthotics.[1] The workflow of the International Committee of the Red Cross (ICRC) has long been considered as the standard to produce prostheses for LMICS.[2-4] Traditional plaster methods are used to perform stump measurements and production of the prostheses socket. These plastered socket shapes are highly dependent on the experience and skills of the prosthetic specialist and this implies difficulty in quality assurance regarding fit and durability.[5,6]
There is an increasing interest in implementing 3D printing technology for health-related problems.[7] A relatively new way to design and produce prosthetic sockets is using computer-aided design (CAD) and computer-aided manufacturing (CAM) systems.[8] Using this technique, the production process could be more consistent and faster. Because, the entire process is automated, the socket fitting would become less dependent on the individual prosthetist’s skills and experience. This could increase the rate of successful prosthetic fitting, especially in LMICS.
Several foundations have been set up to produce customised 3D printed medical aids in LMICs.[9,10] However, because of the limited research and follow-up performed on these projects, it is difficult to assess the quality of the medical aids and the extent to which the projects have been successful and are still ongoing. Scientific research on 3D printed arm prosthetics in LMICs is very limited, and no research has been done on 3D printed prosthetics for lower extremities. As a result, it remains unclear what the potential of these 3D printed prosthetics is and how much impact it has on the quality of life.[11] Below, we describe a 3D project in Sierra Leone in which we aim to provide scientific evidence for our approach in 3D printed prosthetics.
3D lab Sierra Leone
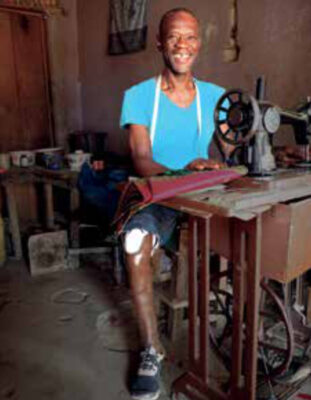
The 3D lab was set up in the Masanga Hospital in Sierra Leone in collaboration with the 3D lab at the Radboud University Medical Centre. The project started in 2018 with a feasibility study to investigate the added value of a 3D printer in a resource-limited healthcare setting. Low-cost 3D printed arm prostheses and other medical aids, such as umbilical cord clamps, braces for patients with scoliosis, and splints to prevent burn contractions were produced.[12] Van der Stelt et al. concluded that aesthetic designs for arm prostheses were just as important as functional designs due to stigmatism of handicapped people. 3D Printed braces were helpful because of the patient-specific design and were produced without many extra costs. In 2020, a clinical study was conducted to test low-cost 3D printed transtibial prostheses. Technical studies were performed, and initial pilot designs were clinically tested on Dutch patients first.[13] Test results showed that the prostheses were sufficiently durable, and after ethical approval had been obtained in Sierra Leone, the prostheses were approved for testing in practical life in Sierra Leone. The short-term results were published in EClinicalMedicine.[14] Patients received several weeks of physical therapy after receiving the prosthesis, and local physiotherapists were trained to provide this training. After six weeks, all participants were still wearing the prosthesis and six out of eight participants reached their personal rehabilitation goals. All of the participants were no longer in need of using crutches thanks to the prosthesis.[14] These studies showed that the design of the socket and aesthetics were of added value regarding both functionality and restoring confidence. Long-term follow-up is required to prove the sustainability of the 3D printed prostheses and improved health related quality of life of patients. The uniqueness of this project is that we aim to provide scientific evidence for our approach. All our study results and clinical outcomes are published in international peer-reviewed scientific journals, which is not often the case with many other projects where prostheses are handed out and patients are not followed up. In addition, we believe it is very important to work together with the local population. Our main goal is to make the project fully independent and sustainable in the future.
Costs and manufacturing time
First, the patient’s stump is 3D scanned in approximately ten minutes. After this, the 3D design of the transtibial socket is created within twenty minutes. Last, it takes approximately twenty hours to 3D print the prosthetic socket. See Figure 1 and 2 for the optical scanning and 3D printing process.

The printing material of the socket costs around US$ 20. The other parts of the prosthesis do not have to be custom-made, standard prosthesis parts can be used for this. See Figure 3 for the prosthesis with 3D printed socket. The prostheses were equipped with a 3D printed aesthetic coverage, so that they resembled a ‘real’ leg in the respective natural skin colour of the individual participant (Figure 4). We currently use imported prosthesis parts that cost a total of US$ 62. The local manufacturing of the prosthetic foot cost US$ 5. The entire material cost of the 3D printed prosthesis is around US$ 87. These costs are low compared to the regular prostheses, which would cost between US$ 100 and US$ 200.



After a two-week rehabilitation process, people can start walking again (see example in Figure 5).
Sustainability
Within the framework of this project, we try to recruit and train as many local staff as possible. This is easy for most manual labour and physiotherapists. However, digitally designing and printing of the prosthesis is still a process that requires specific skills and knowledge, and developing these skills is difficult due to the lack of general IT knowledge. This results in a need for automation of the digital designing process and strategic investment into a structured training programme. The focus for the coming years is on making a simple software programme so that prostheses can be designed and produced in a standardised and automated way by local employees themselves. It is expected that this will make prosthetics less dependent on the skills of the individual prosthetist and enable more people to be trained in a short period of time.
There is a close collaboration with the National Physiotherapy and Rehabilitation Programme in Sierra Leone. In this way, we are trying to implement this technique as much as possible in cooperation with the local authorities. Our goal is to make the project completely independently run by the local population.
Future perspective
Further research on standardisation of the 3D workflow will be performed. Our team has been expanded with several students from the University of Twente, Delft University of Technology and HAN University of Applied Sciences. In the future, we hope to include students from the University in Freetown, Sierra Leone.
Essential elements for sustainable approach are: easy-to-work with 3D software, training of local people, and replacement of the imported prosthetic parts by local products. This will lower the costs of a prosthesis and make the prostheses more financially accessible for the local population.
In the next few years, the foundation intends to provide complete workflow packages for each type of amputation. Each package will consist of a 3D scanner and 3D printer, electricity supply, and an automated software package. This will replace a large workshop to fabricate prostheses; and it would even be possible to create a mobile workshop, so that prosthesis facilities can be available everywhere.
Conclusion
There is an unmet urgent need for prostheses in LMICs. Competitively priced, fully functional prostheses can be locally produced using 3D printing technology and improve the lives of amputees. Apart from helping patients, this project will include a locally driven manufacturing programme that will create qualified jobs.
See for more information and pictures: www.3dsierraleone.com

Other members of ‘Foundation 3D printing in developing countries’:
- Irene Fleur Kramer, MD, PhD, treasurer
- Prof. Thomas Maal, PhD, secretary
- Prof. Martin Grobusch, MD, PhD, board member
References
- World Health Organization, World Bank. World report on disability [Internet]. Geneva: World Health organization; 2011 (accessed 2021 Jul 7). 350 p. Available from: https://www.who.int/disabilities/world_report/2011/report.pdf?ua=1
- Laing S, Lythgo N, Lavranos J, et al. Transtibial prosthetic socket shape in a developing country: a study to compare initial outcomes in pressure cast hydrostatic and patella tendon bearing designs. Gait Posture. 2017 Oct;58:363-8. doi: 10.1016/j.gaitpost.2017.08.017
- Jensen JS, Raab W, Fisk J, et al. Quality of polypropylene sockets for trans-tibial prostheses in low-income countries. Prosthet Orthot Int. 2006 Aprl;30(1):45-59. doi: 10.1080/03093640600568336
- Jensen JS, Nilsen R, Zeffer J. Quality benchmark for trans-tibial prostheses in low-income countries. Prosthet Orthot Int. 2005 Apr;29(1):53-8. doi: 10.10180/17461550500085147
- Nayak C, Singh A, Chaudhary H, et al. An investigation on effects of amputee’s physiological parameters on maximum pressure developed at the prosthetic socket interface using artificial neural network. Technol Heal Care. 2017 Oct 23;25(5):969-79. doi: 10.3233/THC-160683
- Colombo G, Rizzi C, Regazzoni D, et al. 3D interactive environment for the design of medical devices. Int J Interact Des Manuf. 2018;12:699-715. doi: 10.1007/S12008-018-0458-8
- Schonwetter T, Van Wiele B. 3D printing: enabler of social entrepreneurship in Africa? The roles of FabLabs and low-cost 3D printers [Internet]. Cape Town, Ottawa: Open African Innovation Research; 2018. 38 p. Available from: https://openair.africa/wp-content/uploads/2020/05/WP-18-3D-Printing-Enabler-of-Social-Entrepreneurship-in-Africa.pdf
- Kuehn BM. Clinicians embrace 3D printers to solve unique clinical challenges. JAMA. 2016 Jan 26;315(4):333-5. doi: 10.1001/jama.2015.17705
- Victoria Hand Project [Internet]. Victoria: Victoria Hand Project; 2021 [accessed 2020 May 7]. Available from: https://www.victoriahandproject.com/
- Nia Technologies Inc. Niatech [Internet]. Toronto: Nia Technologies Inc; 2018. Available from: https://niatech.org/
- Diment LE, Thompson MS, Bergmann JHM. Three-dimensional printed upper-limb prostheses lack randomised controlled trials: a systematic review. Prosthet Orthot Int. 2018 Feb;42(1):7-13. doi: 10.1177/0309364617704803
- Van der Stelt M, Verhulst AC, Vas Nunes JH, et al. Improving lives in three dimensions: the feasibility of 3D printing for creating personalized medical AIDS in a rural area of Sierra Leone. Am J Trop Med Hyg. 2020 Apr;102(4):905-9. doi: 10.4269/ajtmh.19-0359
- SlideShare [Internet]. 2021. Low-cost 3D printed transtibial prosthetic sockets in a rural area of Sierra Leone. 2020 Jun 27 [accessed 2020 Jul 3]. Available from: https://www.slideshare.net/MerelVanderStelti/lowcost-3dprinted-transtibial-prosthetic-sockets-in-a-rural-area-of-sierra-leone-236295435?qid=d6f24c03-bba4-405f-be8c-df5f9d1bd9fd&v=&b=&from_search=1
- Van der Stelt M, Grobusch MP, Koroma AR, et al. Pioneering low-Cost 3D printed transtibial prosthetics to serve a rural population in Sierra Leone. EClinicalMedicine. 2021 May 8:35:100874. doi: 10.1016/j.eclinm.2021.100874