Main content
| Case An apparent birth defect caused a South Sudanese mother to seek help for her, otherwise healthy, 2-day-old son. An abdominal wall defect was seen just below the umbilical cord (Figure 1). The boy was breastfeeding well, and he passed urine and stool normally. No other signs of congenital abnormalities were found. The treating global health doctor in training asked Consult Online specialists for advice on diagnosis and surgical treatment options. |
Setting
This case was seen in an emergency setting hospital in South Sudan with 150 beds and basic surgical services.
Specialist advice
Within a day, the surgeons of Consult Online responded to the question, saying that a bladder exstrophy was the most likely diagnosis. They stated that unskilled treatment of this condition, which is not immediately life-threatening, might lead to complications, but the upper urinal tract (kidneys and ureters) will not be affected as long as there is a free flow of urine. Attempts to close the bladder can possibly lead to obstruction, which is difficult to handle in this particular hospital. The advice was to transpose the ureters into the sigmoid, with or without a pouch. Since this was not an emergency, it was advised not to intervene until a skilled surgeon would be available. In the meantime, the kidneys needed to be monitored by ultrasound imaging, since dilatation of the ureters or renal pelvis would indicate the need for an intervention. Furthermore, it was considered important to avoid or minimise trauma to the exposed inner surface of the bladder. In the absence of transparent adhesive dressings, clean cotton cloths would be a good alternative to protect against… Antibiotic prophylaxis was considered not necessary.
Follow-up
After two weeks, the mother reported for a follow-up consultation: her son was doing well and there was no hydronephrosis seen on ultrasound examination. However, some granulation tissue had begun to appear (Figure 2). Surgery had not been scheduled yet, since a skilled surgeon was still not available.


granulation tissue had formed.
Background
Bladder exstrophy (exstrophy meaning ‘inversion of a hollow organ’) is a complex congenital disorder within the exstrophy-epispadias complex, which also covers epispadias and cloacal exstrophy. An overdeveloped cloacal membrane, preventing medial migration of mesenchymal tissue, appears to be the cause of the disorder. The incidence is 3-5 cases per 100,000 live births, with boys more likely to be affected than girls. [1]
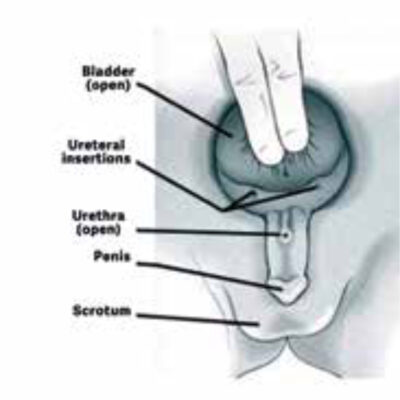
Clinical features
The main characteristics of bladder exstrophy are protrusion and inversion of the urinary bladder through a defect in the lower abdominal wall, with an open exposed dorsal urethra (Figure 3). However, several other organ systems can also be affected. [2] In males, epispadias are seen, and additionally the penis is shortened and the dorsal foreskin is absent. In females, significant genital abnormalities are seen as well. Furthermore, the umbilicus is situated in a more caudal position than normal, lying just above the abdominal wall defect. Outward malrotation of the pelvic bones may lead to diastasis symphysis pubis and consequently separation of the pubic bones, possibly causing an abnormal gait later in life. Another possible complication is faecal incontinence, due to an anteriorly displaced anus, in combination with associated abnormalities of pelvic floor muscles. [2]
Treatment and prognosis
In high-income countries, affected infants undergo repair surgery early in life. [2] Little research has been done concerning management and prognosis of bladder exstrophy in low-resource settings. However, in settings marked by poverty, parental illiteracy, and limited access to health care facilities, first presentations in adulthood do occur. All documented adult cases presented with urine incontinence and had a normal renal function. [3] As can be expected, the risk of urinary tract infections is higher in people with bladder exstrophy.
Urinary diversion (creating a functional connection between the urinary and intestinal tracts) is not being done in high-resource settings anymore. However, if a skilled surgeon is not available or regular follow-up is not possible, it is the treatment of choice. The urine will enter the colon and leave the body via the stool. Even in adults, successful rehabilitation and improved quality of life have been shown to be possible. [3]
Even in adults, successful rehabilitation and improved quality of life have been shown to be possible.
References
- Jayachandran D, Bythell M, Platt MW, et al. Register based study of bladder exstrophy-epispadias complex: prevalence, associated anomalies, prenatal diagnosis and survival. J Urol. 2011 Nov;186(5):2056-2061. DOI:10.1016/j.juro.2011.07.022.
- Borer JG. Clinical manifestations and initial management of infants with bladder exstrophy. UpToDate. Updated 2019 Dec 2. Available from: https://amc-literatuur.amc.nl/f5-w-68747470733a2f2f77777772e7570746f646174652e636f6d$$/contents/clinical-manifestations-and-initial-management-of-infants-with-bladder-exstrophy?search=bladder.
- Venkatramani V, Chandrasingh J, Devasia A, et al. Exstrophy-epispadias complex presenting in adulthood: a single-center review of presentation, management, and outcomes. Urology. 2014 Nov;84(5):1243-1247. DOI:10.1016/j.urology. 2014.06.063.

















































