Main content
The Otto Kranendonkfonds (OKF) (Fund) was established as a foundation in 1994 under the name of Stichting Erefonds Tropische Geneeskunde (Honorary Fund Tropical Medicine Foundation), later also called Stimuleringsfonds (Stimulation Fund). The purpose of the OKF is to stimulate scientific research and knowledge transfer in the area of global health (including tropical medicine) by members of the Netherlands Society for Tropical Medicine and International Health (NVTG). The fund provides grants to studies in line with sustainable development goal 3 (“ensuring healthy lives and promoting well-being for all at all ages”), with a specific focus on low- and middle-income countries (LMICs) or low-resource settings [1] The fund typically supports operational research conducted by clinicians and researchers at the start of their careers.
History
The fund was an initiative of the late prof. dr. Otto Kranendonk, after his retirement as extraordinary professor in tropical health sciences at the University of Amsterdam, and director of the department of Tropical Hygiene at the Royal Tropical Institute in Amsterdam. He donated stock market shares to the NVTG with the intention that the annual dividend (profit) would be used to support research, without affecting the total value of the investment. In reality this has not always worked out, since there have been episodes of stagnation or even declines of the investment, which precluded the granting of subsidies. While initially the benefactor preferred to remain anonymous – hence the name Stimuleringsfonds – one of his grandchildren later expressed the desire to rename the fund in honour of his late grandfather. Since 2011 the fund has been known under the name Otto Kranendonkfonds.
Types of research that are (co-)funded
Since the establishment of the fund, quite a number of research projects have been funded, many in the field of maternal health, others on infectious diseases such as tuberculosis, HIV and malaria, and more recently on a wider range of global health topics (Table 1). The majority of the projects resulted in one or more scientific publications. Three of them have so far contributed to PhD dissertations.
A recent journal article by Mooij et al. listed global health research published by Dutch medical doctors in global health and tropical medicine in LMIC (not limited to OKF funded studies) and explored the evidence generated. [2] It identified eighteen PhD theses successfully completed by medical doctors in global health and tropical medicine over the past thirty years. More than half of these involved maternal health and obstetrics, and the majority of the studies were conducted in low-income countries, mostly in rural hospitals, involving more than seventy local co-authors. The authors conclude that expatriate physicians are in a unique position to conduct scientific research in an LMIC setting, in addition to their clinical and other tasks. This brings added value, often in terms of health service quality improvement and strengthening local research capacity.
Application procedures and criteria
The Science Committee of the NVTG evaluates applications for OKF funding and advises the NVTG Board. Criteria for application can be obtained from the NVTG secretariat. Unfortunately, there has been no financing available to fund any studies since the beginning of this year (2020).
Conclusion
The OKF has played a modest but successful role in supporting research by NVTG members and their colleagues in LMICs. It stimulates health professionals to undertake operational studies and for some juniors it has boosted a career in health research. Some of the subsidised projects have been part of a PhD trajectory. The application process is relatively simple and quick, although funding opportunities are rather erratic. We encourage those of you who are out “in the field” or have plans to work abroad to look out for future calls for proposals on the NVTG website or in the newsletter.
| YEAR | NAME APPLICANT | RESEARCH TITLE | RELATED PUBLICATIONS | PHD YEAR |
|---|---|---|---|---|
| 1998 | Patrick van Rheenen | The use of paediatric tuberculosis scorecard in an HIV-endemic area in Zambia | Van Rheenen P. The use of the paediatric tuberculosis score chart in an HIV-endemic area. Trop Med Int Health. 2002 May;7(5):435-41. | – |
| 2001 | Marjan Hoexum | Maternal mortality, Nicaragua | – | – |
| 2001 | Marieke Lagro | Postnatal follow-up and problems in the postpartum period, Zambia | Lagro M, Liche A, Mumba T, Ntebeka R, van Roosmalen J. Postpartum health among rural Zambian women. Afr J Reprod Health. 2003 Dec;7(3):41-8. PMID: 15055145. Lagro M, Liche A, Mumba T, Ntebeka R, van Roosmalen J. Postpartum care attendance at a rural district hospital in Zambia. Trop Doct. 2006 Oct;36(4):205-8. | – |
| 2002 | Peter Petit and Patricia Buijtels | Tuberculosis research in Zambia | Unknown | – |
| 2003 | Marita Nijenhuis | Chloroquine efficacy in pregnant women in a rural area in Zambia where HIV-prevalence is high | Unknown | – |
| 2003 | Jeroen van Dillen | Therapeutic efficacy of chloroquine and sulfadoxine-pyrimethamine in Onandjokwe Hospital, Northern Namibia And: Malaria diagnosis using automated detection of malaria pigment in Northern Namibia | Van Dillen J, De Jager AJ, De Jong I, Wendte JF. Overdiagnosis of malaria in hospitalized patients in Namibia. Trop Doct. 2007 Jul;37(3):185-6. de Langen AJ, van Dillen J, de Witte P, Mucheto S, Nagelkerke N, Kager P. Automated detection of malaria pigment: feasibility for malaria diagnosing in an area with seasonal malaria in Northern Namibia. Trop Med Int Health. 2006 Jun;11(6):809-16. | 2009 |
| 2003 | Patrick van Rheenen | Delayed cord clamping as an intervention to reduce infant anaemia in a malarious area in Zambia | van Rheenen P, de Moor L, Eschbach S, de Grooth H, Brabin B. Delayed cord clamping and haemoglobin levels in infancy: a randomised controlled trial in term babies. Trop Med Int Health. 2007 May;12(5):603-16. | 2007 |
| 2004 | Eveline Geubbels | ? | – | – |
| 2008 | Heleen van Beekhuizen | Treatment of retained placenta with misoprostol: a double blink randomized placebo controlled study | van Beekhuizen HJ, Pembe AB, Fauteck H, Lotgering FK. Treatment of retained placenta with misoprostol: a randomised controlled trial in a low-resource setting (Tanzania). BMC Pregnancy Childbirth. 2009 Oct 23;9:48. van Beekhuizen HJ, Tarimo V, Pembe AB, Fauteck H, Lotgering FK. A randomized controlled trial on the value of misoprostol for the treatment of retained placenta in a low-resource setting. Int J Gynaecol Obstet. 2013 Sep;122(3):234-7. | – |
| 2010 | Ed Zijlstra | Survey of the management and complications of diabetes mellitus in Malawi | Cohen DB, Allain TJ, Glover S, Chimbayo D, Dzamalala H, Hofland HW, Banda NP, Zijlstra EE. A survey of the management, control, and complications of diabetes mellitus in patients attending a diabetes clinic in Blantyre, Malawi, an area of high HIV prevalence. Am J Trop Med Hyg. 2010 Sep;83(3):575-81. Glover SJ, Burgess PI, Cohen DB, Harding SP, Hofland HW, Zijlstra EE, Allain TJ. Prevalence of diabetic retinopathy, cataract and visual impairment in patients with diabetes in sub-Saharan Africa. Br J Ophthalmol. 2012 Feb;96(2):156-61. | – |
| 2011 | Yadira Roggeveen | Innovative partnerships for safe motherhood: participation and trans-disciplinary collaboration as tools towards increasing skilled birth attendance | Roggeveen Y, Birks LK, van Kats J, Manyama M, Hatfield JM, Bunders JFG, Scheele F & van Roosmalen J. Low utilization of skilled birth attendants in Ngorongoro Conservation Area, Tanzania: a complex reality requiring action. Health Vol.5 No.7D, July 18, 2013. http://dx.doi.org/10.4236/health.2013.57A4011 | Expected |
| 2011 | Remco Peters | Epidemiology of chlamydia and gonorrhoea in women in Mopani District, South Africa | Peters RP, Dubbink JH, van der Eem L, Verweij SP, Bos ML, Ouburg S, Lewis DA, Struthers H, McIntyre JA, Morré SA. Cross-sectional study of genital, rectal, and pharyngeal Chlamydia and gonorrhoea in women in rural South Africa. Sex Transm Dis. 2014 Sep;41(9):564-9. Dubbink JH, de Waaij DJ, Bos M, van der Eem L, Bébéar C, Mbambazela N, Ouburg S, Peters RP, Morré SA. Microbiological Characteristics of Chlamydia trachomatis and Neisseria gonorrhoeae Infections in South African Women. J Clin Microbiol. 2016 Jan;54(1):200-3. | – |
| 2013 | Reinou Groen | Traumatic injuries in Sierra Leone | Stewart KA, Groen RS, Kamara TB, Farahzad MM, Samai M, Cassidy LD, Kushner AL, Wren SM. Traumatic injuries in developing countries: report from a nationwide cross-sectional survey of Sierra Leone. JAMA Surg. 2013 May; 148(5):463-9. | – |
| 2013 | Sybrich Tiemersma | Delayed cord clamping in South Africa | Tiemersma S, Heistein J, Ruijne R, Lopez G, van Lobenstein J, van Rheenen P. Delayed cord clamping in South African neonates with expected low birthweight: a randomised controlled trial. Trop Med Int Health. 2015 Feb;20(2):177-83. | – |
| 2014 | Floris Braat | Maternity waiting home to improve maternal and neonatal outcome in the Gurage Zone, Southern Ethiopia (Butajira General Hospital) | Windsma M, Vermeiden T, Braat F, Tsegaye AM, Gaym A, van den Akker T, Stekelenburg J. Emergency obstetric care provision in Southern Ethiopia: a facility-based survey. BMJ Open. 2017 Nov 8;7(11):2018459. doi: 10.1136/bmjopen-2017-018459. Braat F, Vermeiden T, Getnet G, Schiffer R, van den Akker T, Stekelenburg J. Comparison of pregnancy outcomes between maternity waiting home users and non-users at hospitals with and without a maternity waiting home: retrospective cohort study. Int Health. 2018 Jan 1;10(1):47-53. Vermeiden T, Braat F, Medhin G, Gaym A, van den Akker T, Stekelenburg J. Factors associated with intended use of a maternity waiting home in Southern Ethiopia: a community-based cross-sectional study. BMC Pregnancy Childbirth. 2018 Jan 19;18(1):38. | – |
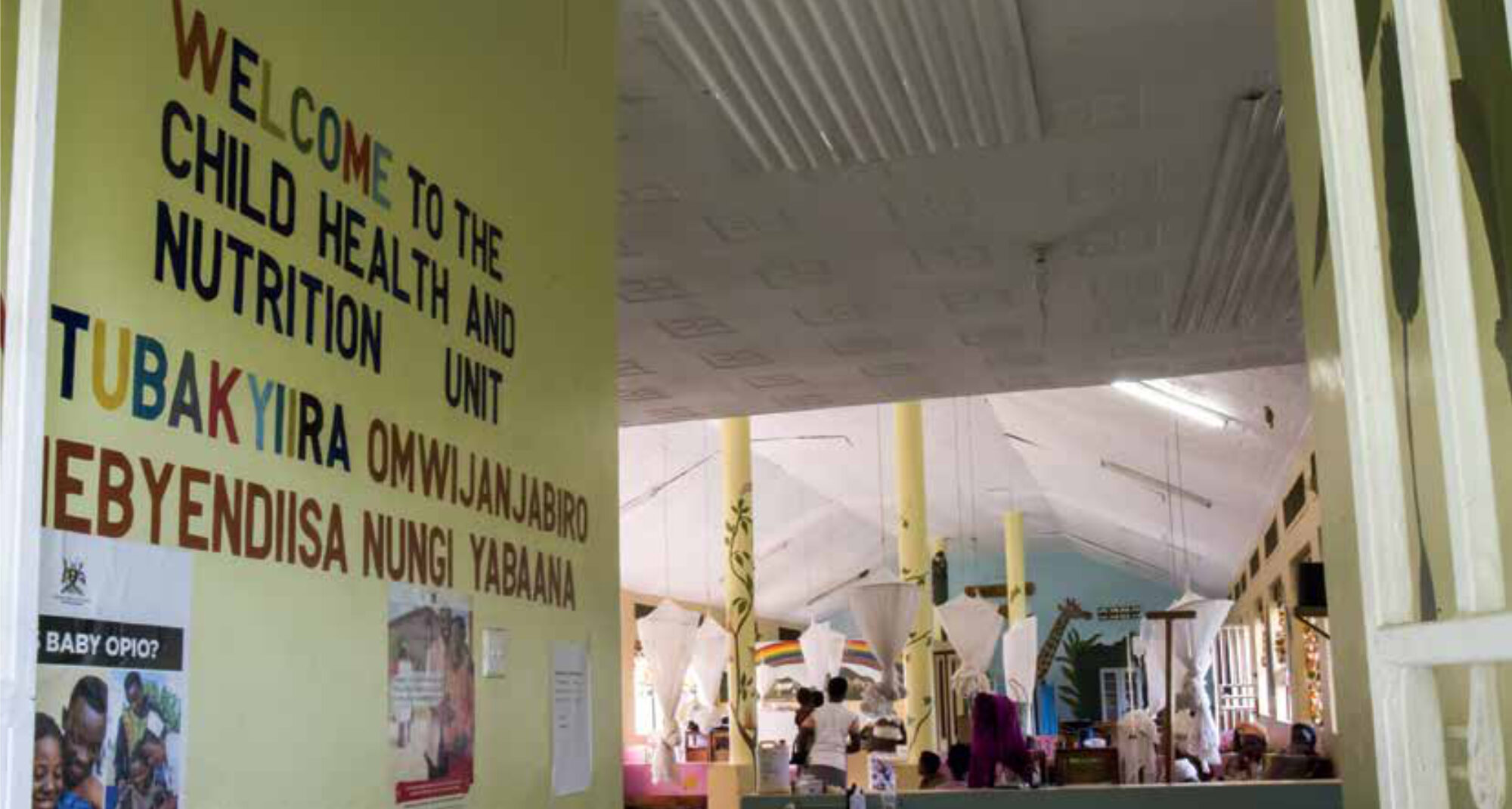
| 2014 | Barbara Nolens | Outcomes of vacuum extraction at Mulago Hospital, Uganda | Nolens B, Lule J, Namiiro F, van Roosmalen J, Byamugisha J. Audit of a programme to increase the use of vacuum extraction in Mulago Hospital, Uganda. BMC Pregnancy Childbirth. 2016 Sep 2;16(1):258. Nolens B, Namiiro F, Lule J, van den Akker T, van Roosmalen J, Byamugisha J. Prospective cohort study comparing outcomes between vacuum extraction and second-stage caesarean delivery at a Ugandan tertiary referral hospital. Int J Gynaecol Obstet. 2018 Jul;142(1):28-36. | – |
| 2016 | Alinda Vos | Unmasking a silent killer: diabetes care in HIV-patients in a rural medical clinic in South Africa | In process | – |
| 2017 | Thom Hendriks | Evaluation of a quality assured in-service training in surgical treatments for burns at Haydom Lutheran Hospital (Mbulu, Manyara, Tanzania) | Unknown | – |
| 2017 | Natasha Housseine | The development of a simple decision-making tool for optimal allocation of intra-partum care in low-income countries. | Unknown | – |
| 2018 | Benjamin Jelle Visser | A pragmatic approach to treat podoconiosis in Ethiopia | Article in press | – |
| 2018 | Elena Ambrosino | Urogenital infections and pregnancy in Pemba Island (Zanzibar, United Republic of Tanzania) | Juliana NC. Deb S. Ouburg S. Chauhan A. Pleijster J. Ali, S.M.; Morré, S.A.; Sazawal, S.; Ambrosino, E. The Prevalence of Chlamydia trachomatis and Three Other Non-Viral Sexually Transmitted Infections among Pregnant Women in Pemba Island Tanzania. Pathogens 2020, 9, 625. Two other manuscripts in preparation. | – |
| 2018 | Hanna Mathéron | Prevalence and pathogen identification of peri-partum infections in Sierra Leone | In preparation | Expected |
| 2018 | Jonathan H. Vas Nunes | Wounds in Sierra Leone; a knowledge, attitude and practice study | In preparation | Expected |
| 2019 | Anneloes Eleveld | Evaluation of access to care, incidence and outcome of treatment of patients with fractures of the lower extremities in Haydom Lutheran Hospital (Tanzania) | In preparation | – |
| 2019 | Dickens Oyango | Validity of urine dipstick for routine assessment of adherence to isoniazid preventive therapy (IPT) among children living with HIV (CLHIV) in Western Kenya | In preparation | – |
References
- NVTG [Internet]. Wijhe: Nederlandse Vereniging voor Tropische Geneeskunde en Internationale Gezondheidszorg; 2020. Otto Kranendonkfonds; 2020. Available from: https://www.nvtg.org/wat-we-doen/otto-kranendonk-fonds
- Mooij R, Jurgens EM, van Dillen J, et al. The contribution of Dutch doctors in Global Health and Tropical Medicine to research in global health in low- and middle-income countries: an exploration of the evidence. Trop Doc. 2020 Jan;50(1):43-49. DOI: 10.1177/0049475519878335