Main content
Ebola virus disease is caused by five distinct, yet closely related viruses. The Ebola virus group belongs to the filoviridae family, constituting an important class within the causative agents of the viral haemorrhagic fever group of diseases. We will briefly discuss the epidemiology of Ebola virus disease, highlighting the current ongoing outbreak in West Africa, and briefly touch upon pathophysiology, clinical features, prevention, containment as well as current and future treatment options.
Epidemiology
Ebola virus disease is caused by five distinct but closely related viruses, with four of them originating from Central Africa and Zaire ebolavirus being responsible for the majority of outbreaks to date and being considered the most virulent of the Central African strains [1]. Together with Marburg virus, the Ebola virus group belongs to the Filoviridae family, constituting an important group within the causative agents of the viral haemorrhagic fever group of diseases.
The first recorded outbreaks of Ebola virus disease which led to the identification of the Ebola viruses took place almost simultaneously in 1976, in both Uganda and Zaire (now the Democratic Republic of Congo, DRC) [1,2]. During those and the subsequent (almost 30) outbreaks on record [2] until the recent events in West Africa changed the game completely, the basic pattern always seems to follow similar chains of events. Regularly, the outbreak would begin somewhere in a remote rainforest area, with a group of hunters venturing into the forest, hunting and slaughtering a primate such as a chimpanzee or gorilla (or a range of other bush meat sources such as antelope). Part of the animal would be eaten during the hunting trip; and days after their return to their village, one or several of the hunters would fall ill, with all or most of them succumbing to the disease within days. Following ritual burials, whose preparations would possibly lead to intense contact with the body and bodily fluids of the deceased by several (up to many) people, secondary and then tertiary cases would start to crop up. In due course, authorities would be notified, and outbreak control teams would move into the area, sealing off the afflicted village or region. The outbreak would come to an end after having killed between 40 to 90% of the patients; usually several dozens of people up to more than 200 (with a maximum of 224 deaths amongst 425 sick people recorded in Uganda in 2000) [3]. The survival rates would be increasing towards the end of an outbreak when medical assistance would become available, and after the virus would have been passed on to a second, third and maybe fourth generation of patients, following the initial zoonotic transmission step; with very few deaths amongst the latter generations of patients and an increasing number of apparently healthy infected individuals turning seropositive.
This basic pattern has been broken (whilst there was a concomitant smaller outbreak in 2014 in a remote region of the DRC [4]) with the current, still ongoing eruption of Zaire Ebola virus disease in West Africa; where the virus surfaced 1000s of kilometers away from its ‘classical’ habitat and geographic location in the greater Central African rainforest belt region. Towards the end of 2013, a rapidly increasing number of cases of what turned out to be Ebola virus disease (with a clinical picture featuring intractable watery diarrhoea as main characteristic, rather than the frank bleedings in severely diseased individuals leading to the baptizing of Ebola as a viral haemorrhagic fever) [5] hit Guinea [6,7], with further cases rapidly emerging from the neighbouring countries of Liberia [7] and Sierra Leone [7,8]. Only several months into this outbreak, the full dimension of the outbreak was recognized [6]. By that time, cases had spilled over to Senegal [9], Nigeria [9] and Mali [9] yet were contained by the respective authorities and responsibly acting health care workers in an unprecedented effort. As well, first cases of repatriated/evacuated health care workers were recorded in Europe and the USA. At the time of writing, at the beginning of February 2015 and about 14 months into the outbreak, 22,525 cases and 9,004 deaths (as of 6 February) have been reported from those three countries, with the brunt being borne by Sierra Leone [10]. Few additional cases have been recorded in North America and Europe (none on other continents) [11-13]; Mali, Senegal and Nigeria have been declared Ebola-free, and incident case numbers are falling rapidly and steadily in Guinea and Liberia, and now also in Sierra Leone, in reverse order of the evolution of the outbreak.
Transmission
Transmission to man in the first zoonotic step in the transmission chain before human-to-human (often nosocomial transmission) would occur, was for long thought to be confined to bush meat sources, mainly primates. What became clear soon was that another main (primary) animal reservoir existed, as primates were obviously disease-prone themselves. For many years, the search for the primary host (initially focusing on rodents as main suspects) was puzzlingly unsuccessful, until various fruit bat species were identified as virus reservoir [1]. With regard to the ongoing outbreak, it was the fruit bat reservoir (either through consumption of infected animals as bush meat or through consumption of what fruit bats had feasted on before) that is considered as the primary outbreak source now in West Africa.
Pathophysiology
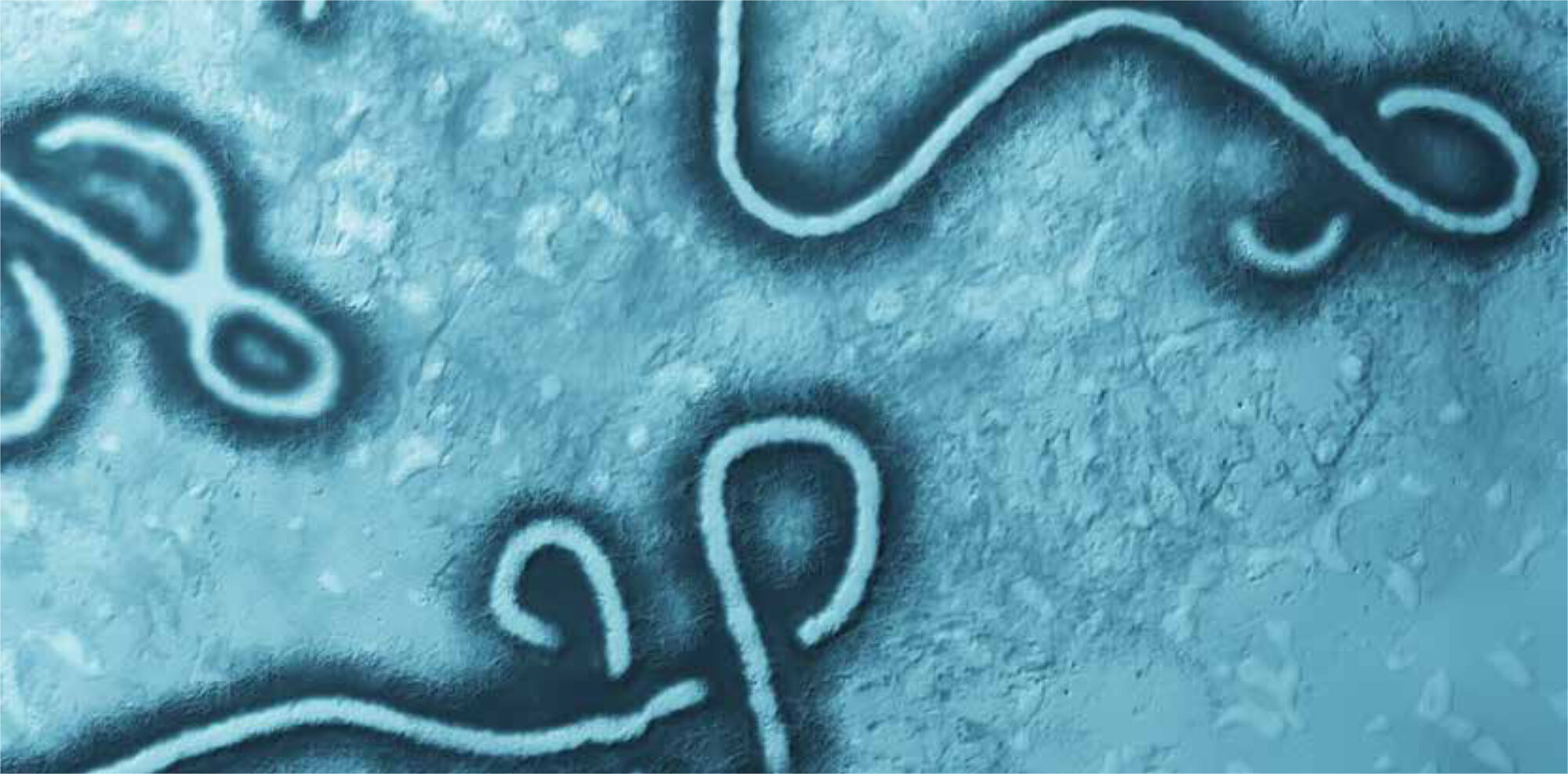
The structure of the filoviridae is simple, with a protein shell encasing the viral genome. The outer surface of the virus is dotted with 195-kD glycoprotein spikes, which on contact fuse with human cell membranes, preferably dendritic cells. After membrane fusion, the viral genome is integrated into the host genome, and massive viral replication in all host tissues enfolds [1]. Destruction of the host organs leads to multi organ failure and very frequently to internal and external bleedings in due course, with bacterial sepsis as a common complication at late stage disease [1].
Disease and differential diagnosis
In the early stage of disease, following an incubation period of 2-21 days (in a small proportion of patients, this may be prolonged) signs and symptoms are unspecific, often mimicking a flu-like illness. Sudden onset of fever, prostration, headache and throat pain, myalgias and arthralgias, possibly a generalized rash and gastrointestinal symptoms such as diarrhoea (initially or consistently non-bloody, as characteristic for the ongoing outbreak rather than frank bleedings), nausea, and vomiting may be followed by a rapid deterioration of the patient, with multi organ failure, internal and external bleedings, and (hypovolaemic/haemorrhagic) shock ensuing. Death occurs frequently, mostly with Zaire Ebola virus, and more at the beginning of an outbreak rather than towards its end; which may be in part owed to the proposed decline of virulence through human-to-human passage, and in part to improved medical care at the end of an outbreak [1,5,6,8].
The differential diagnosis is broad and encompasses malaria, bacterial sepsis (often a complication in later stages of Ebola virus disease), typhoid fever, leptospirosis, rickettsiosis, amoebiasis, and many others; as well as – with few characteristic features attributable only to a number of cases, such as orchitis in men; few reliable clinical features indicating a diagnosis of Ebola rather than other locally endemic VHFs (such as lassa fever or yellow fever).
Laboratory diagnosis
A standard laboratory test would be an ELISA to determine antibody levels (IgM, then IgG) from early on in the disease. However, the current gold standard is diagnosis by RT-PCR. The one main challenge is the development of reliable, rapid POC tests; the other is the problem of the extreme contagiousness of blood and other bodily fluids, which renders laboratory personnel (particularly in unsuspected cases) at highest risk of infection, and which has led to the high safety level requirement for specimen handling.
Treatment – established and experimental
To date, there is no established specific therapy. Main element of warranting survival of patients is early recognition, aggressive rehydration, low-threshold antibiotic therapy to control concomitant bacterial sepsis, and empirical antimalarial treatment in unconfirmed Ebola cases. The chances for survival are determined not only by the virulence of the infecting strain but also by host factors, time lapse between onset of symptoms and initiation of supporting therapeutic measures, and in general to the level of access to routine intensive care measures including organ-supportive therapy such as mechanical ventilation and haemodialysis [1,11-13].
However, a wide range of experimental therapies [14] had been tested earlier in often very small cohorts of monkeys, indicating efficacy, and which are now being fast-tracked through early stages of clinical development with the goal of being made available once proven safe and once available in the large quantities required. Amongst the various therapeutic approaches, monoclonal antibodies against viral surface structures are the most promising. There is also renewed interest in the administration of reconvalescent serum to patients with active disease, based mainly on anecdotal evidence; it is obvious how difficult it will be to conduct a controlled high-standard phase III trial on this or any other method within an outbreak situation.
Prophylaxis, prevention and hygiene measures required to contain Ebola
To date, there is no marketed vaccine, which would be safe, effective, efficacious and ready to be administered on a mass scale in order to curb the ongoing outbreak. However, not dissimilar to a range of specific therapeutics, a number of vaccine candidates (with several prototypes involving viral vectors carrying gp195 fragment encoding RNA into the host cells in the lead) is currently fast-tracked in public-private partnership efforts through phase I safety and immunogenicity trials in Europe, the USA and Africa). For the time being, disease prevention through early recognition of ongoing transmission and transmission risk on individual level is paramount. Avoidance of contact with bodily fluids (sweat, semen remaining virus-positive weeks after cure of infected males) is key to containment of the disease. Key to successful containment is early patient recognition in and outside the epidemic setting, discouragement (if unavoidable with reinforcement) of unsafe cultural (bush meat consumption, traditional burial practices) and hygienic practices, strict hygiene protocol adherence including (safe usage and disposal of) protective clothing and equipment and consumables, strict laboratory safety measure implementation and isolation of patients [15] (Figures 1, 2).
Outlook
Academic institutions around the world (such as the Dutch University Medical Centers) have braced themselves to contain Ebola in the case of suspect patients presenting themselves unexpectedly, or being referred as suspect or confirmed cases; as well as that there was a firm, although delayed outbreak response in the hard-hit West African region. With the likelihood of this outbreak trailing on at low level for years, or the disease becoming endemic and having to be accounted for continuously in the near future in the general differential diagnosis of the febrile patient, a sustained, concerted, long-term effort of the international community, both political and financial, is required to regain control over Ebola virus disease on a global scale.

During the ongoing outbreak, the LHMC continues to operate as a local hospital, maintaining basic health care services, whilst a part of the hospital has been set apart and fitted out as a holding centre for patients suspected of ebolavirus infection.

Meticulous attention to safety and hygiene protocols in endemic settings as well as in overseas centres caring for repatriated suspected and confirmed Ebola cases is the key to contain an outbreak and to prevent nosocomial spread.
References
- Feldmann H, Geisbert TW. Ebola haemorrhagic fever. Lancet 2011;377:849-62.
- Del Rio C, Mehta AK, Lyon GM 3rd, Guarner J. Ebola Hemorrhagic fever in 2014: The tale of an evolving epidemic. Ann Intern Med 2014;161:746-8.
- http://www.who.int/mediacentre/factsheets/fs103/en [last accessed on 9 February 2015]
- Maganga GD, Kapetshi J, Berthet N, et al. Ebola virus disease in the Democratic Republic of Congo. New Engl J Med 2014;371:2083-91.
- Chertow DS, Kleine C, Edwards JK, et al. Ebola virus disease in West Africa – Clinical manifestations and management. N Engl J Med 2014;371:2054-7.
- Bah EI, Lamah MC, Fletcher T, et al. Clinical presentation of patients with ebola virus disease in Conakry, Guinea. N Engl J Med 2015;372:40-7.
- WHO Ebola Response Team. Ebola virus disease in West Africa – the first 9 months of the epidemic and forward projections. N Engl J Med 2014;371:1481-95.
- Schieffelin JS, Schaffer JG, Goba A, et al. Clinical illness and outcomes in patients with ebola in Sierra Leone. N Engl J Med 2014;371:2092-100.
- http://www.who.int/csr/don/archive/disease/ebola/en [last accessed on 9 February 2015]
- http://apps.who.int/gho/data/view.ebola-sitrep.ebola-summary-20150206/en [last accessed on 9 February 2015]
- Kreuels B, Wichmann D, Emmerich P, et al. A case of severe ebola virus infection complicated by gram-negative septicaemia. New Engl J Med 2014;371:2394-401.
- Lyon GM, Meeta AK, Varkey JB, et al. Clinical care of two patients with ebola virus disease in the United States. New Engl J Med 2014;371:2402-9.
- Wolf T, Kann G, Becker S, et al. Severe ebola virus disease with vascular leakage and multiorgan failure: treatment of a patient in intensive care. Lancet December 19, 2014 [epub ahead of print].
- De Clercq E. Ebola virus (EBOV) infection: Therapeutic strategies. Biochem Pharmacol 2015;93:1-10.
- Missair A, Marino MJ, Vu CN, et al. Anesthetic implications of ebola patient management: a review of the literature and policies. Anesth Analg Dec 30, 2014 [epub ahead of print].
Figure 1. Health care workers preparing for entering the Ebola isolation ward in full Personal Protection Equipment (PPE) at the Lion Heart Medical Centre (LHMC) in Yele, Tonkolili District in Northern Province, Sierra Leone.
During the ongoing outbreak, the LHMC continues to operate as a local hospital, maintaining basic health care services, whilst a part of the hospital has been set apart and fitted out as a holding centre for patients suspected of ebolavirus infection.
Figure 2. Desinfection and exit area of the Ebola isolation ward at the LHMC, Yele, Sierra Leone.
Meticulous attention to safety and hygiene protocols in endemic settings as well as in overseas centres caring for rep